 |
|
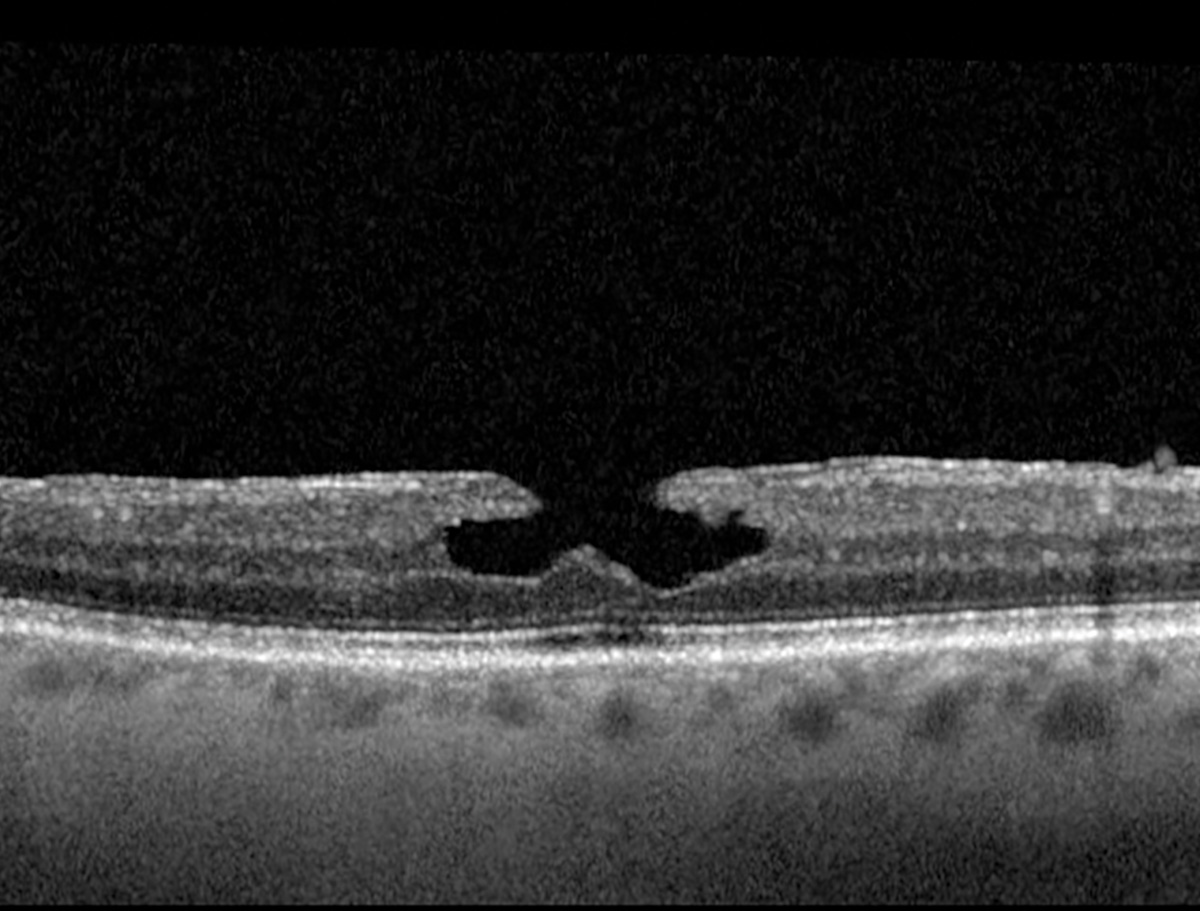
The degenerative subtype of LMH displayed a larger FAZ area, lower parafoveal and perifoveal superficial capillary plexus vessel densities and lower foveal deep capillary plexus vessel densities. Photo: Jessica Haynes, OD. Click image to enlarge. |
Lamellar macular holes (LMHs) are often characterized by defects in the inner retinal layers. Two distinct types of LMH, tractional and degenerative, have been identified based on structural differences observed in OCT imaging. The tractional form displays schisis-like separation of the neurosensory retina between the outer plexiform and outer nuclear layers, often with an intact ellipsoid layer and associated tractional epiretinal membranes, while the degenerative type features round-edged cavitation, a foveal bump and LMH-associated epiretinal proliferation.
Researchers in Turkey recently evaluated OCT angiography (OCT-A) findings in the degenerative and tractional subtypes of LMH. They found that microvascular changes between the two highlight their distinct pathologies and support recent changes in the classification and terminology of LMHs.
This study, which was published in Journal of Ophthalmology, included 17 patients with the degenerative subtype, 18 who had the tractional form of LMH and 20 healthy individuals as the control group. The foveal avascular zone (FAZ) and retinal vascular densities in the superficial, deep capillary and choriocapillary plexuses were analyzed and compared with those of fellow eyes and healthy controls using OCT-A.
The mean FAZ area was wider in the degenerative subtype (0.33mm2) compared to the tractional subtype (0.24mm2) and control eyes (0.26mm2). Foveal vessel densities in the superficial and deep capillary plexuses were lower in the degenerative group than in the tractional group, (21.7% vs. 26.8% and 28.5% vs. 36.9%). Choriocapillary vascular density in the parafoveal area was also lower in degenerative lamellar macular holes compared to the tractional group (60.4% vs. 63.7%). Compared to controls, eyes with degenerative and tractional LMH showed lower vessel densities in the parafoveal and perifoveal areas of the superficial and deep capillary plexuses, as well as all layers of the chroiocapillary plexus. In the foveal area, the LMH groups showed higher foveal vascular density (FVD) in the superficial capillary plexus than control eyes, while in the deep capillary plexus, FVD was lower in the degenerative LMH eyes relative to the other groups.
“The distinct vascular features identified in the two subtypes of LMH imply that they are different clinical entities,” the study authors wrote in their paper. “These parameters may serve as biomarkers for disease progression.”
They noted that further research with a larger sample size examining retinal vascular changes would significantly enhance our comprehension of LMH.
Gültekin BP, Kalaycı D. Evaluation of optical coherence tomography angiography in degenerative and tractional lamellar macular hole. J Ophthalmol. July 19, 2024. [Epub ahead of print]. |


