 |
|
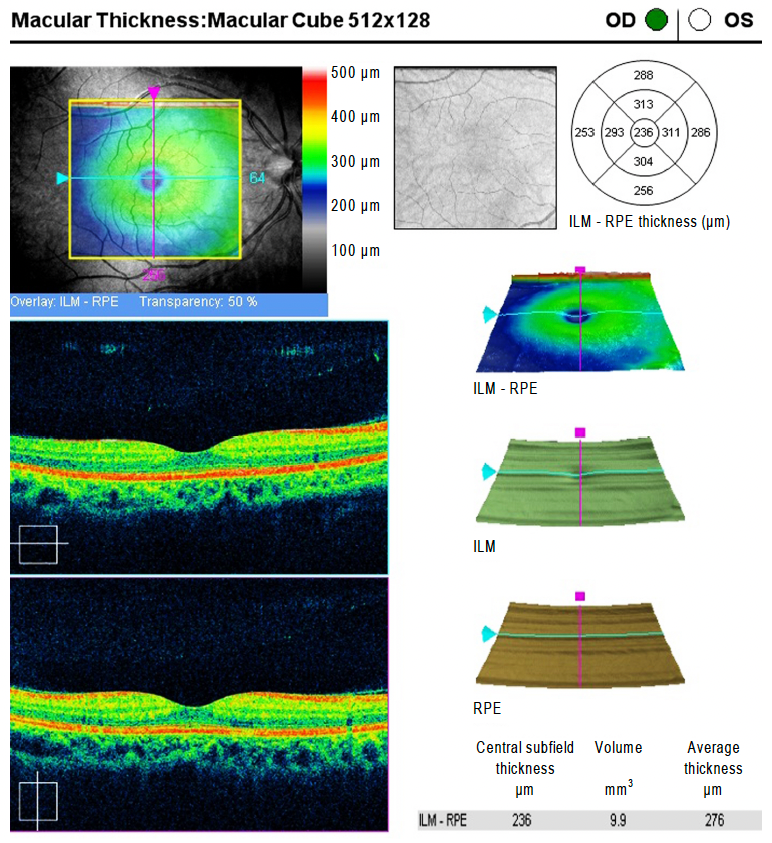
A new study takes a deeper dive into the connection between genetics and disease risk, particularly the role blood type plays in retinal structure indices. Researchers discovered macular thicknesses were significantly higher in participants from the AB blood group, compared to others. They also found that blood type B participants were more likely to have peripapillary RNFL thinning than other blood groups. The authors believe blood type should be considered in the clinical interpretation of retinal structures, but more studies are warranted. Photo: Kang NH, et al. J Korean Ophthalm Soc. Click image to enlarge. |
Various studies have found a connection between genetics and retinal diseases, while others have suggested a genetic relationship in the retinal structural parameters themselves. Considering that one’s genetic pool determines blood type, researchers of a new study published in BMC Ophthalmology sought to explore the potential influence this factor may have on structural indices such as peripapillary retinal nerve fiber layer (RNFL) thickness and macular thickness. According to their findings, macular thicknesses were significantly higher in participants in the AB blood group, but blood type B was correlated to a decreased global and sectoral peripapillary RNFL thickness in the superior and inferior quadrants.
The cross-sectional study sample included 328 participants from a tertiary referral eye hospital in Tehran. Of these, 219 subjects were women and the mean age of participants was 63.3 years. Participants were excluded from the study if they had a history of genetic or systemic diseases affecting the retina and optic nerve. Along with analyzing ABO blood groups, this study also looked at Rh blood groups. In addition to the findings regarding the higher average macular thickness found in blood type AB, average macular thickness was significantly thinner in Rh+ compared to the Rh– group.
Blood type B was related to a decreased global and sectoral peripapillary RNFL thickness in both the superior and inferior quadrant, contrasted with blood type AB, which was associated with a decreased peripapillary RNFL thickness in the superior quadrant. Blood type O showed thicker global peripapillary RNFL thickness, as well as superior and inferior peripapillary RNFL thickness, compared to other ABO blood groups.
The study authors hypothesized that the thicker fovea in individuals with blood type AB could be due to a genetic link, and cited other epidemiological studies that have shown racial differences in macular thickness, namely Causasians, Asians and Africans. “Apart from the genetic link, differences in some biochemical characteristics between different blood groups may also contribute to this finding,” they wrote.
One unique aspect of this study is that none of its participants had a history of retinal disease. “To our best knowledge, this is the first study to examine the relationship between blood groups and peripapillary RNFL thickness in a healthy population,” they said, and went on to mention previous research that included blood type and glaucoma risk. In those studies, researchers found relationships between blood type B and the disease. “By combining the findings of the present study and previous reports, it can be concluded that a thinner peripapillary RNFL in people with blood type B may make them more susceptible to glaucomatous damage,” wrote the authors of this new study. “Therefore, the association between glaucoma and blood type B may be rooted in the optic nerve structure. This association may be due to a genetic link as peripapillary RNFL thickness has been shown to have a relatively high heritability.”
These findings could have important implications in the clinic, continued the authors. “Since macular thickening is an important diagnostic sign of macular disease, it is recommended that blood type be considered in the clinical interpretation of macular thickness, especially in people with blood type AB, to avoid misdiagnosis,” they wrote. Second, “considering inherent peripapillary RNFL thinning, one should be cautious in interpreting abnormal reports in individuals with blood type B to avoid false positive diagnoses of optic neuropathy.” Third, people with type B blood may be more susceptible to peripapillary RNFL loss and advanced glaucomatous damage from inherently thin anatomy here, “so it is logical to be more careful in the clinical management of these patients in terms of follow-up periods and IOP control.”
Researchers say they tried to effectively control for confounding factors in the study, but noted the hospital-based nature of the study reduces its generalizability, and the sampling method may have added bias. Also, “as the study was performed in an elderly population, the conclusions may not be applicable to other age groups,” they wrote.
Although this study found a direct correlation between macular thickness in participants with type AB blood, and an inverse correlation in peripapillary RNFL thickness in blood type B, the authors recommend larger trials to determine if these findings may be incidental.
Shanbezadeh E, Vasaghi-Gharamaleki B, Nabovati P, et al. Analysis of macular thickness and peripapillary retinal nerve fiber layer thickness in various ABO and Rh blood groups. BMC Ophthalmol. July 24, 2024. [Epub ahead of print.] |


