 |
|
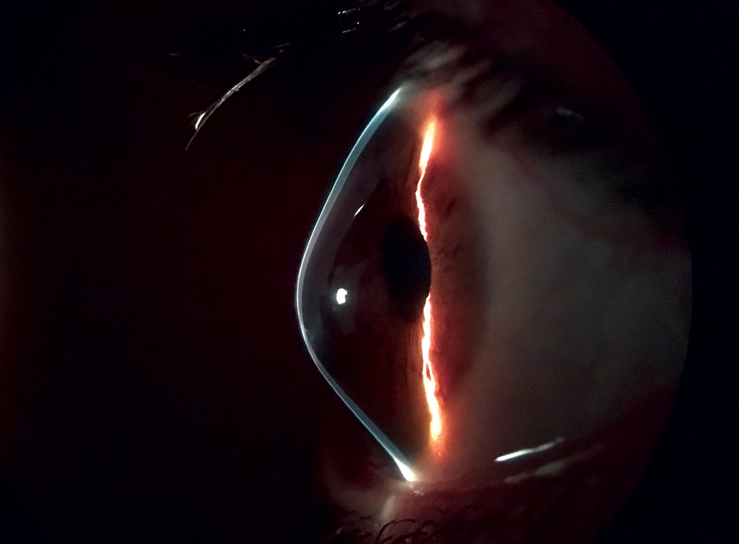
Patients described reduced QoL in plain-language answers that described how poor vision and healthcare access difficulties had cascading effects on everyday scenarios, offering more insight into how keratoconus truly affects their lives. Photo: Brian Chou, OD, and Jerome Legerton, OD. Click image to enlarge. |
The distorted and unstable vision that keratoconus patients experience, typically from a young age and consistently from then on, can have serious effects on quality of life (QoL). Due to the condition’s potentially debilitating nature, a team of Australian researchers wanted to better understand and characterize the impact that keratoconus has on patients’ daily lives. Their results were published last week in the British journal Eye.
Patients diagnosed with keratoconus were recruited from the Sydney Eye Hospital and were interviewed in a semi-structured, in-depth way both in person and over the phone. These interviews were meant to provide thematic analysis of overarching QoL domains affecting these patients.
Among the 33 patients included, median age was 37, ranging from 18 to 65 years, and the majority were male (75.8%). After analyzing the 2,551 quotes obtained from the interviews, analysis revealed seven broad themes of QoL impact and subsequent lingering anxieties: driving difficulties (7.8% of patient comments), career setbacks (10.2%), the inconvenience of chronic visual symptoms (25.4%), limits on enjoyment of hobbies (5.8%), strained personal relationships (9.8%), financial hardships (4.1%) and healthcare fears and frustrations (34.5%).
Not surprisingly, most references described a negative relationship between the condition and the seven aforementioned domains. More specifically, common QoL issues recorded were frustration with treatment efficacy, fear of disease progression, inconvenience with contact lenses, forced career changes and job loss, cost of contact lenses and feelings of isolation and discrimination.
Candid Comments From PatientsIn the study described here, researchers interviewed a range of keratoconus patients about the disease’s impact on various aspects of daily life. Below is a sampling of patient comments (edited for clarity and brevity); many more are available in the full study, available by open access here. “I got to a point where I ended up withdrawing from university just because I didn’t feel like I could properly analyze the data to finish off the thesis.” “I’ve done a lot of lateral transfers at work as opposed to moving up the chain just because I feel like with more responsibility you have a larger and larger budget to manage. And it’s reading those numbers and dealing with numbers that I worry about.” “It’s almost wasting your money because every six months you’re going to have to buy new hard contact lenses and with your eyes getting worse and worse it’s just going to be very expensive.” “If I have to use a computer, my face is basically plastered up against the screen, and I hate that because it looks stupid.” “When I go out with my friends, I cannot look at the menu to order anything.” “If we have a really rainy, dark, cold day, I’m not going to go because I don’t want to drive.” “The biggest problem is mobility. You’ve got to rely on unreliable public transport.” “I try not to take the highways as often. I try to take smaller back streets and roads.” “Sometimes it drains your motivation to go out and go to an event. You kind of just want to lay down and close your eyes and not have to worry about anything.” |
The authors expand upon these qualifiers in their discussion. Emotional strain and perceived inefficiency were mapped onto healthcare experiences, while both visual and non-visual symptoms impeded patients’ daily lives and required coping mechanisms. Life opportunities were limited by education and careers being affected, with enjoyment of normal life being limited by the condition as well. This is further elucidated through patients reporting feelings of isolation, misunderstanding and guilt. Independence was constrained due to limitations on driving and financial burdens.
One previous investigation has described keratoconus to have an impact disproportionate to its clinical severity because of the young age at which patients are affected. This was also reflected in the current study, with individuals describing feeling manifecting at a critical stage in life when they are unable to bear the financial costs of the condition and its treatment as well as beginning careers, romantic relationships and having no prior surgery experience. Concerns with self-image were also present in the current study.
Another interesting observation was that the patients of this study had difficulty using digital screens, needing to take adaptive measures like increasing font size, increasing contrast and using larger monitors. Given the ubiquity of digital devices in modern life, this alone will prove to be a frequent source of frustration for keratoconic patients.
In their paper, the investigators suggested that their study identified unique QoL domains impacted in keratoconus patients across a range of differing clinical and lifestyle scenarios and that these insights “can contribute to the development of robust keratoconus-specific QoL questionnaires, improve clinician understanding or patients’ experiences and inform the development of new treatments.”
Fan L, Kandel H, Watson SL. Impacts of keratoconus on quality of life: a qualitative study. Eye (Lond). July 23, 2024. [Epub ahead of print]. |


