When assessing optic nerve damage for detecting glaucoma, peripapillary retinal nerve fiber layer (RNFL) thickness and ganglion cell complex (GCC) are among the quintessential biomarkers. However, a new study published in Journal of Clinical Medicine considered the differences in OCTA-derived macular vessel density (VD) biomarkers in early to moderate primary open-angle glaucoma patients. They discovered a significantly reduced global, hemispheric and quadrant superficial capillary plexus (SCP) VD in the whole image, parafovea and perifovea, signaling that this metric may be just as useful in early detection of POAG as RNFL and GCC thickness.
 |
|
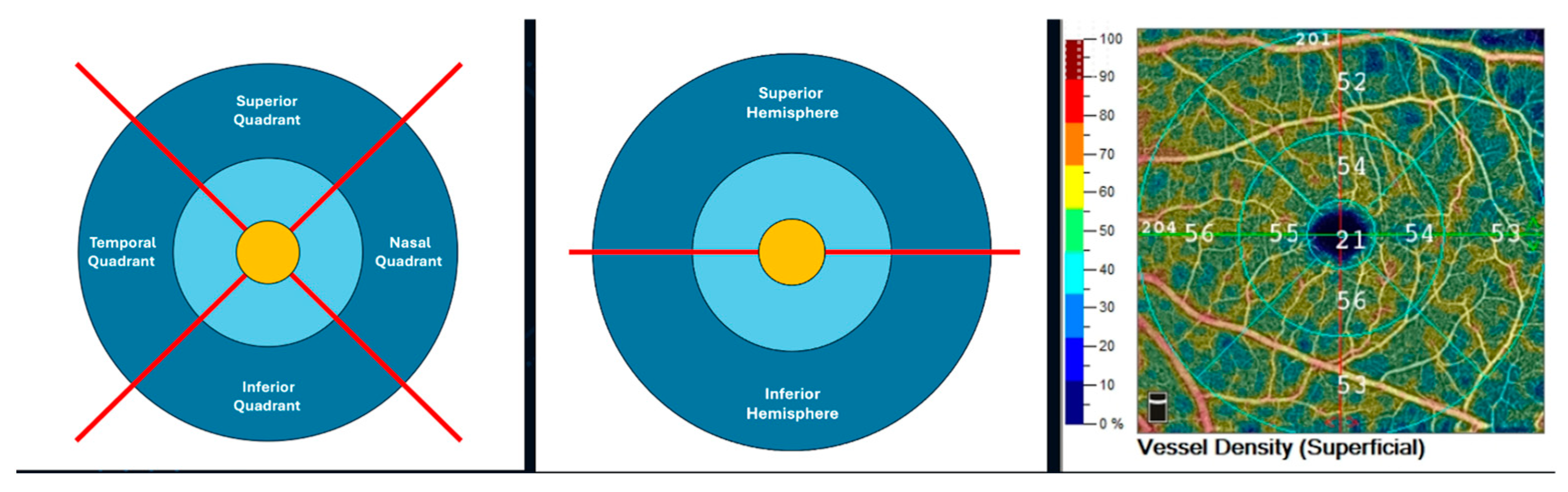
A new study looked at the relationship between global and regional OCT-A- macular biomarkers and their role in early-stage glaucoma detection. It found that superficial capillary plexus vessel density was significantly lower in POAG patients, which correlated to an increasing functional severity based on visual field data. This measure could also be equated with the accuracy of RNFL and GCC thickness in the diagnosis of POAG, wrote the authors. Photo: Vercellin AV, et al. J Clin Med. July 18, 2024. Click image to enlarge. |
This study included 56 POAG patients and 94 non-glaucomatous controls, all of whom underwent OCTA assessment for VD in the SCP, deep capillary plexus (DCP), foveal avascular zone (FAZ) and flow area in the outer retina and choriocapillaris. Researchers excluded anyone in the “advanced” and “very advanced” stages, instead focusing on early-stage disease metrics. In the POAG patients, SCP VD was significantly lower with increased functional disease severity for the whole image and for several perifoveal regions, which agrees with previous findings that a loss of SCP VD may first occur in the perifovea region of the macula in patients with early disease. SCP VD in the whole image and perifovea were significantly lower in POAG patients in stage 2 than stage 0. No significant differences between POAG patients and controls for FAZ parameters, DCP VD, and the retinal and choriocapillaris flow area were found.
“In clinical practice, often only the global (average) values of structural and vascular biomarkers are analyzed and used to make therapeutic decisions,” wrote the authors in their paper. “However, global values within normal limits may hide regional hemodynamic or structural damage that may lead to disease progression in glaucoma eyes.” This stresses the importance of novel approaches that assess not only global values of OCT-A macular biomarkers but also their regional levels in terms of hemispheres/quadrants and parafovea/perifovea, the researchers explained in their paper.
“This study is among the first to quantify macular VD at the level of the SCP and DCP at a global, hemispheric, and quadrant level and to evaluate differences between POAG patients and controls in structural and hemodynamic parameters in the FAZ as well as in the outer retinal layer and the choriocapillaris,” they continued.
Authors of this study also demonstrated the diagnostic accuracy of SCP vessel density in the whole image as being significantly higher than DCP density. It was also similarly accurate to global RNFL and GCC thickness. “Our results agree with previous studies that show GCC thickness and macula VD had similar diagnostic accuracy to discriminate preperimetric early glaucoma,” they wrote.
The relatively small sample size was one limitation of the study acknowledged by the authors. “Future studies with an increased number of study participants may possibly allow for some of the comparisons to reach statistical significance,” they wrote. Results were statistically adjusted for age, since the POAG patient group was significantly older than the control group, and the authors also adjusted for systemic hypertension and diabetes mellitus to limit the effect of these confounding factors and excluded any participant with ocular complications that may have affected their results.
“In this analysis, we found that SCP VD was significantly lower in POAG patients compared to non-glaucomatous controls,” they summarized in the journal article. “In addition, there was a correlation between SCP VD and increasing functional severity based on visual field data.” The measure had the highest performance among all OCT-A macular vascular biomarkers and was statistically similar to RNFL and GCC thickness for diagnosing POAG, they stated, indicating its viability as a vascular biomarker “that could be used to detect glaucoma in the early stages of the disease in combination or as an alternative to RNFL and GCC thickness.”
Vercellin AV, Harris A, Oddone F, Carnevale C, Siesky BA, Arciero J, Fry B, Eckert G, Sidoti PA, Antman G, et al. Diagnostic capability of OCTA-derived macular biomarkers for early to moderate primary open angle glaucoma. J Clin Med. July 18, 2024. [Epub ahead of print.] |


