 |
Mapping the corneal epithelium in Sjögren’s patients would offer a potential opportunity for eyecare providers to closely monitor disease progression and guide treatment decisions, as well as providing insights into its underlying mechanisms. Photo: Carl Zeiss Meditec. Click image to enlarge. |
Dry eye disease is highly prevalent, and the autoimmune disease Sjögren’s syndrome accounts for about 11% of this patient population. While various devices and measurements have been proven effective in diagnosing dry eye, many of these techniques have not been studied on patients with Sjögren’s, one example being corneal epithelial mapping. Thus, investigators from the University of Pennsylvania wanted to characterize patterns of corneal epithelial thinning measured by AS-OCT in this subgroup of dry eye patients to look for possible associations.
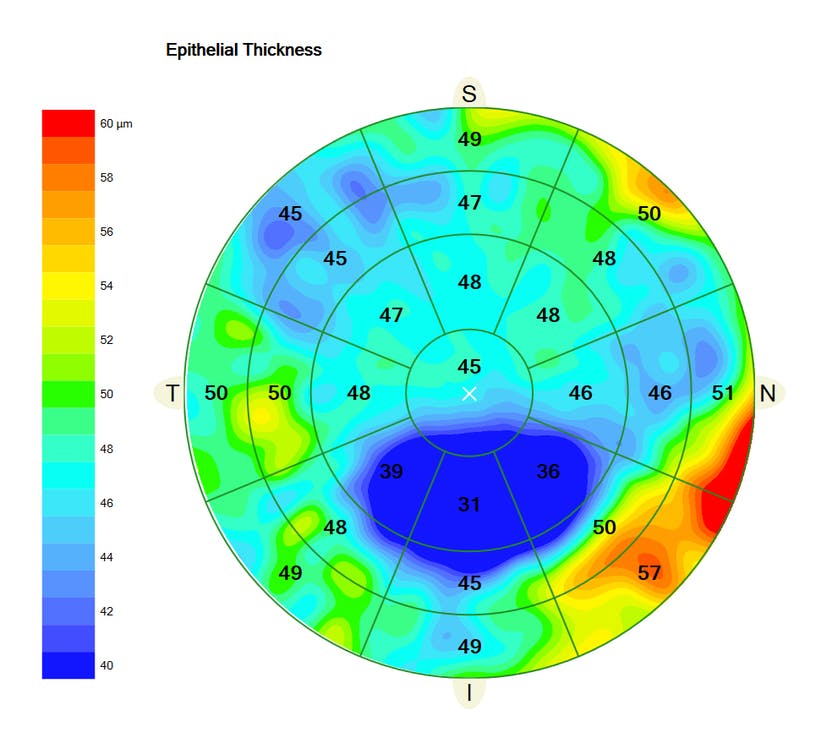
The retrospective review included patient demographics of unanesthetized Schirmer’s test, serologic markers and symptoms measured by the Ocular Surface Disease Index. Corneal epithelial thickness (CET) from both eyes was measured using AS-OCT at the central 3mm and concentric 5mm, 7mm and 9mm zones for superior, temporal, inferior and nasal corneal quadrants.
A total of 15 Sjögren’s patients—all women—were included with a mean age of 58.4 years. What researchers found was that Sjögren’s patients had a significantly thinner superior corneal epithelium, averaging 47.7µm, compared with the inferior epithelium, averaging 53.1µm. What’s more, the epithelial thickness was inversely correlated with Schirmer results, suggesting that an overall CET variability correlates with decreased aqueous tear production and/or secretion, which has not been reported previously. Serologic marker positivity was not associated with any CET measures.
From these results, the authors broadly state, “This pilot study suggests that there is significant superior vs. inferior thinning of corneal epithelium in Sjögren's patients.” Upon discussion, the authors relay this similarly reflects the observation that superior corneal epithelial thinning has been implicated to be the first affected area in dry eye disease patients. Specifically, this study documented that 62.1% of eyes had a superior corneal epithelial thickness of <50µm. This cutoff of <50µm has previously been described in the literature to provide an 81% sensitivity and 79% specificity in differentiating dry eye patients from healthy individuals.
Even further, the superior quadrant thickness was thinner at each concentric zone, and, on average, thinner than the inferior quadrant by 5.4µm. As an explanation, the authors relay that “the superior cornea has been suggested to be more prone to damage due to the frictional forces from eyelid blinking, which may be more pronounced in dry eye patients. It has also been proposed that the central corneal epithelium could be spared due to its distance from the limbus and relatively greater immune privilege.”
The researchers add that “further, larger studies that include various subpopulations of dry eye disease patients are needed to better understand the relationship of CET with objective and subjective measurements of dry eye disease.”
Nguyen BJ, Gupta AS, He J, et al. Corneal epithelial thickness in Sjogren’s disease: a pilot study. Clin Ophthalmol. 2024;2024(18):2175-82. |


