 |
|
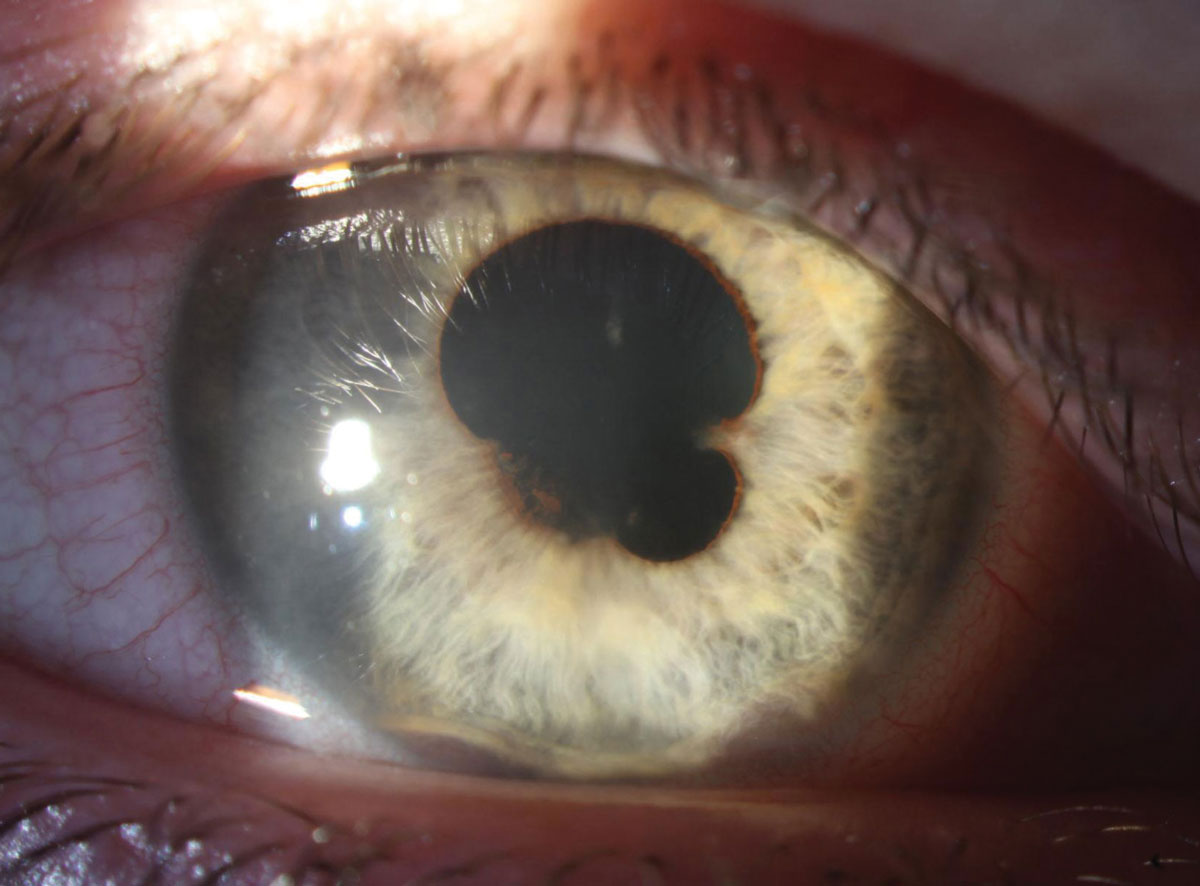
When compared to cytotoxic agents and immune checkpoint inhibitors, treatment with BRAF inhibitors led to a 7.52-fold and 5.68-fold higher risk of uveitis among patients with melanoma and lung cancer. Just over three-quarters of cases (77.8%) and 100% of severe ones occurred within 160 days after drug administration. Photo: Aaron Bronner, OD, and Alison Bozung, OD. Click image to enlarge. |
New research suggests that patients with melanoma or lung cancer who undergo treatment with BRAF inhibitors have significantly higher risk of noninfectious uveitis when compared to patients who receive conventional cytotoxic drugs or immune checkpoint inhibitors. There are three drugs in this class: vemurafenib (Zelboraf), dabrafenib (Tafinlar) and encorafenib (Braftovi).
These findings, published last week in American Journal of Ophthalmology, underscore the importance of educating patients on BRAF inhibitor–associated uveitis risk to ensure prompt evaluation and treatment if symptoms arise.
In this nationwide, population-based, retrospective clinical cohort study, researchers used the Health Insurance Review and Assessment Service database of South Korea to define 77,323 patients with skin melanoma or lung cancer who received BRAF inhibitor therapy (n=396), immune checkpoint inhibitors (n=22,474) or conventional cytotoxic chemotherapy (n=54,453). They then calculated the one-year cumulative incidence of noninfectious uveitis in each patient cohort from the first day of BRAF inhibitor, immune checkpoint inhibitor or cytotoxic agent treatment.
Data revealed that the during the first year of treatment initiation, the cumulative incidence of uveitis among patients who received BRAF inhibitors, immune checkpoint inhibitors or cytotoxic agent treatment was 2.27% (nine cases), 0.35% (79 cases) and 0.33% (242 cases), respectively. The risk of uveitis increased 7.52-fold and 5.68-fold in the BRAF inhibitor–exposed group when compared to the patients who received cytotoxic agents and immune checkpoint inhibitors.
A crossover analysis within the BRAF inhibitor cohort showed a 3.71-fold increase in uveitis risk during one-year post index date in comparison with one-year prior to index date, according to the research team’s findings. The investigators also found that female sex, chronic kidney disease and melanoma were associated with a trend of increased uveitis risk among patients in the BRAF inhibitor group.
“Patients with melanoma or lung cancer undergoing BRAF inhibitor treatment exhibited a significantly elevated risk of noninfectious uveitis compared to those treated with conventional cytotoxic drugs or immune checkpoint inhibitors,” the study authors noted in their recent AJO paper.
“The results of our study emphasize the importance of providing thorough pretreatment education on the potential risk of BRAF inhibitor-associated uveitis to patients receiving BRAF inhibitors, especially for those who have been diagnosed with skin melanoma,” they concluded. “Such education would prompt seeking of ophthalmic evaluation and treatment in case of symptom occurrence during drug administration.”
Jung H, Kim S, Lee C, et al. Real-world incidence of incident noninfectious uveitis in patients treated with BRAF inhibitors: a nationwide clinical cohort study. Am J Ophthalmol. July 6, 2024 [Epub ahead of print]. |


