 |
|
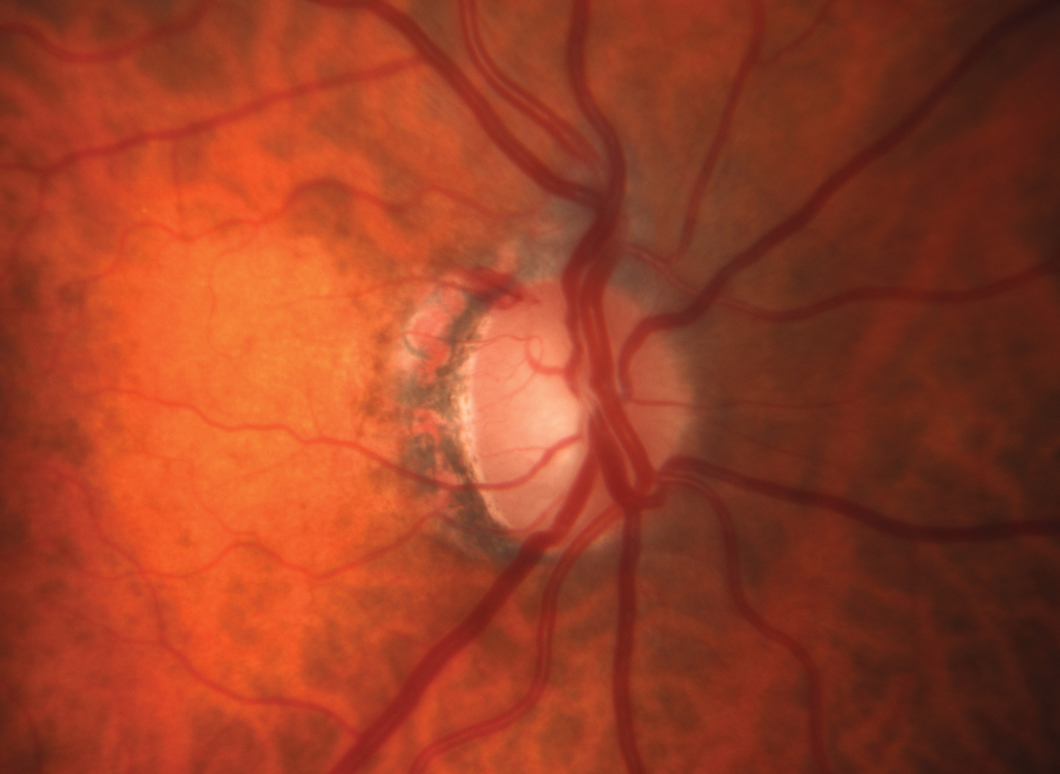
Unsupervised, at-home, multi-day glaucoma testing using two devices resulted in the capture of higher maximum IOPs than in the clinic and good MD correlation of VR visual field testing with HFA. Photo: Michael Chaglasian, OD. Click image to enlarge. |
Telehealth is increasingly looked at as a way to improve glaucoma screening and long-term monitoring. The recent introduction of remote physiologic monitoring devices can continue to build workflows within eyecare that do not rely on clinic time. Given that the healthcare environment is beginning to financially support remote chronic disease monitoring, researchers at Stanford recently designed and conducted a pilot study on 15 glaucoma patients (mean age 60.2) to assess the feasibility, repeatability and validity of unsupervised, at-home visual field testing using a head-mounted visual field tester (Olleyes, VisuAll) and a self-tonometry device (iCare Home). They found that patients are motivated and capable of performing both perimetry and tonometry unsupervised at home, which could potentially supplement in-office testing to expedite treatment decisions.
Participants were trained to use the two devices devices before conducting self-tests at home over consecutive days. At-home IOP measurements were collected four times daily per eye and visual field testing was performed once daily. The results were compared with one in-clinic Humphrey Field Analyzer (HFA) visual field test performed on the day of device training, iCare Home measurements as performed by the trainer and the patient’s last five Goldmann applanation tonometry (GAT) results.
Of the 15 enrolled participants, 62.5% adhered to this schedule for three consecutive days and 60% (nine patients) completed the study. The six excluded participants could not self-measure IOP, particularly those with central visual field loss. The researchers noted that the device could be less useful for more advanced glaucoma patients.
There was a significant correlation between the average mean deviation (MD) values of the at-home visual field tests and the in-clinic HFA test. Additionally, the average of the sensitivities in five of the six Garway-Heath sectors were significantly correlated. The Olleyes VisuAll test duration was also shorter than in-clinic HFA testing. Finally, at-home tonometry yielded statistically similar values compared with trainer-obtained iCare Home values. The mean and range of at-home tonometry were also statistically similar to those for in-clinic GAT, but at-home tonometry demonstrated higher maximum IOP values.
“In our study, the iCare Home on average agreed with the in-clinic iCare Home and GAT measurements but captured statistically significantly higher pressures that were not visible in the clinic, suggesting that at-home testing during or outside of office hours may provide information to physicians that could warrant a change in care or further evaluation, based on clinical judgment, as seen in other studies,” the study authors wrote in their paper for Translational Vision Science & Technology.
“With the increasing affordability, ease of use and portability of these devices, it is likely that they will become more widely used in glaucoma management,” they concluded.
Berneshawi AR, Shue A, Chang RT. Glaucoma home self-testing using VR visual fields and rebound tonometry vs. in-clinic perimetry and Goldmann applanation tonometry: a pilot study. Transl Vis Sci Technol. 2024;13(8):7. |


