 |
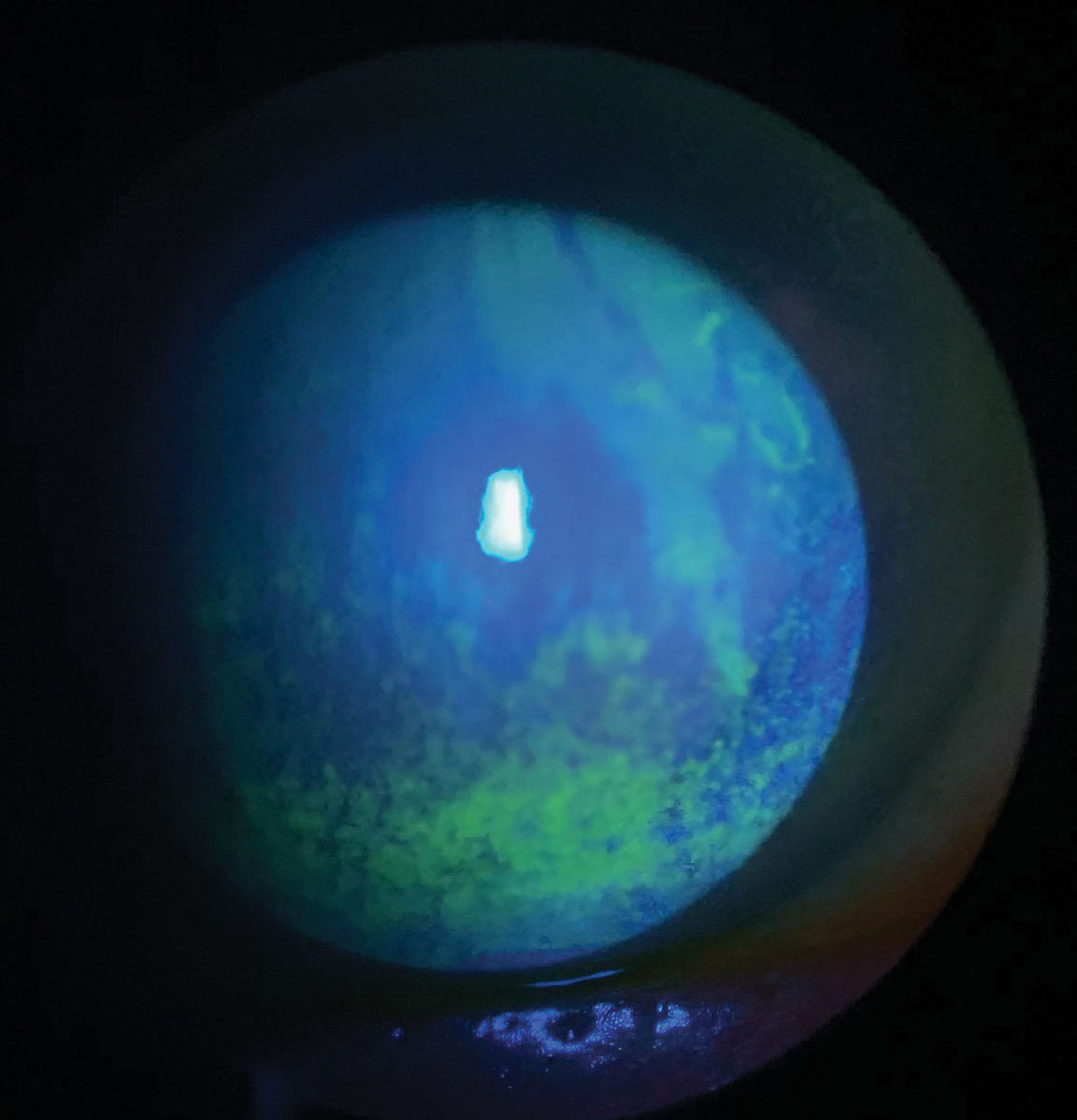
| A greater emphasis should be placed on explaining to patients how environmental and behavioral modifications might mitigate DED. Photo: Scott G. Hauswirth, OD. Click image to enlarge. |
Although prescription treatments for dry eye disease (DED) often improve clinical signs, they may be less effective against patient-reported symptoms, at least initially. In large surveys, clinicians and patients have ranked environmental and behavioral modifications among the most important DED-related research priorities. A new questionnaire-based study sought to investigate the barriers to and facilitators of these modifications by dry eye patients in the United States, as well as how their use may be impacted by socioeconomic status. The researchers found that socioeconomic status does not play a factor, and in regard to environmental and behavioral modifications patients most frequently use are taking breaks to rest eyes, increasing water intake and using hot/cold compresses.
The authors conducted an anonymous online survey of 754 adults with DED living in the United States. Most were aged 18 to 49 years (67%), female (68%) and white (76%) and reported dealing with DED for less than five years (67%).
They found that the environmental and behavioral modifications that patients most frequently use are taking breaks to rest eyes, increasing water intake and using hot/cold compresses. Participants reported a high degree of willingness to consider modifications that they had not tried.
“However, two of the three most frequently used modifications (increasing water intake and using hot/cold compresses) are inexpensive modifications,” the authors noted in their article on the survey.
It is also notable that sizable percentages of respondents (26% to 68%) were currently using the various modifications.
“The most frequently noted biggest barriers pertained to difficulty/inconvenience of modifications and lack of family/employer/social/community support,” the authors explained. “Facilitators of the most frequently used modifications were belief that they work, ease of use/performance, recommendation by providers and affordability.”
To their surprise, socioeconomic status does not seem to be related to barriers to and facilitators of the use of environmental and behavioral modifications for managing dry eye disease-related symptoms.
“Although one may hypothesize that individuals with financial insecurity or in underpaid jobs may have less flexibility in taking breaks to rest their eyes, we did not observe socioeconomic status–related differences in the frequency with which respondents reported taking breaks to rest eyes or the extent to which they experienced barriers to or facilitators of doing so.”
Lastly, for various specific modifications, a sizable percentage of respondents (15% to 39%) reported that they had never tried but would be willing to try them. The authors suggest that this may represent opportunities for health care providers to educate individual patients regarding environmental and behavioral modifications that may be effective for their specific circumstance.
“Greater emphasis should be placed on making patients aware and explaining to them how these modifications might (or might not) mitigate DED-related symptoms,” the authors concluded. “Employers and members of patients' support systems (e.g., family members) should be guided regarding how best to support patients in managing symptoms of dry eye disease.”
Saldanha I, Petris R, Ifantides C, et al. Patient barriers and facilitators for making environmental and behavioral modifications for dry eye in the United States. Optom Vis Sci. December 20, 2023. [Epub ahead of print]. |


