The increasing sophistication of OCT technology continues to reveal associations between posterior segment changes and a variety of neurological disorders. While OCT has already been involved in examining multiple sclerosis (MS) patients, data on MS patients using OCT angiography (OCT-A) is scarcer. Consequently, researchers from Poland wanted to investigate OCT-A measurements and if any could be a useful tool in differentiating rheumatic disorders (RD) from MS.
 |
|
Morphological changes present in rheumatic disease patients’ vasculature includes capillary loss, capillary shape changes, hemorrhages and avascular areas. Photo: Jessica Haynes, OD. Click image to enlarge. |
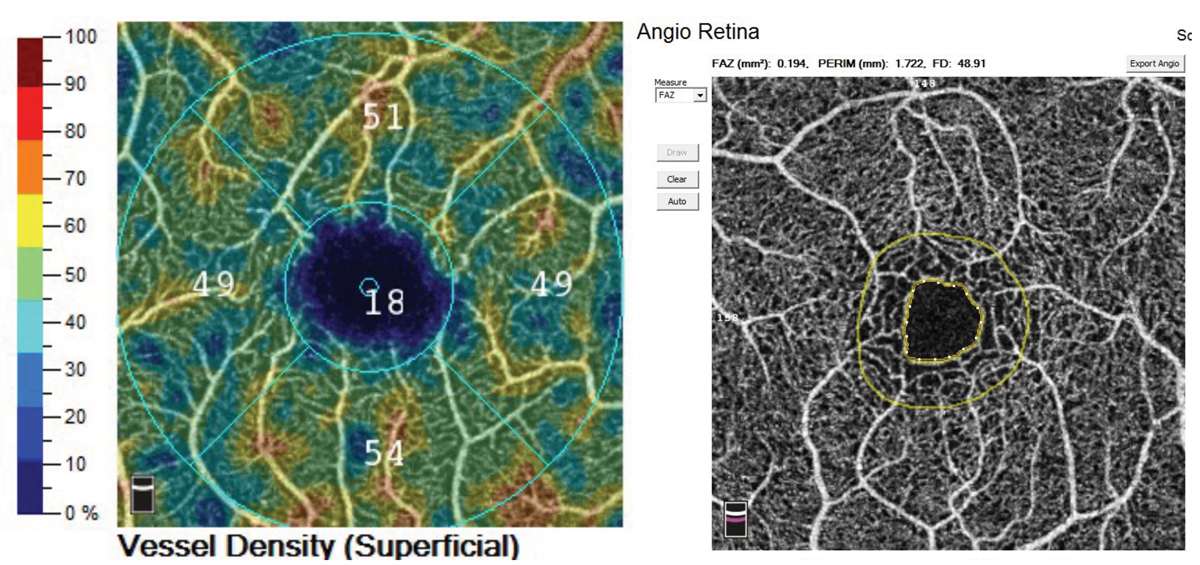
Included in the study was a total of 85 patients—41 had MS, 21 had RD with central nervous system (CNS) involvement and 23 were healthy controls. All underwent OCT-A, with each of the following parameters being measured separately in each eye: average foveal and parafoveal vessel density (VD), average foveal and parafoveal vessel length, of the superficial capillary plexus (SCP) and deep capillary plexus, are, perimeter and circularity of the foveal avascular zone.
The only notable result was that OCT-A showed a VD reduction in the foveal region of the SCP of RD patients’ eyes when compared with MS patients. Otherwise, there were no significant differences in any of the other parameters assessed, including average VD and total average vessel length in the foveal area of the SCP and the deep capillary plexus in controls, MS and RD groups.
Because of this difference, the study authors relay “our results suggest that an OCT-A finding of decreased VD in the foveal region of the SCP may be considered as a potentially useful biomarker of RD in comparison with MS patients.” This counters current research which found that, so far, spectral domain OCT cannot distinguish any specific biomarkers between MS patients vs. those with CNS involvement with RDs.
The researchers discuss how current literature existing on OCT-A and MS patients is not consistent. One study MS patients with optic neuritis history had lower VD in the SCP and deep capillary plexus compared with controls; another found that relapsing-remitting MS patients without optic neuritis history had lower VD in the SCP compared with controls.
The decrease in average VD values in the foveal region of the RD group echoes that of some previous investigations, with previous research finding that those with systemic lupus erythematosus also display a VD decrease of the SCP on OCT-A in addition to an increase in iris vessels flow and foveal avascular zone enlargement.
More generally, the authors extend their findings to potential clinical implications, arguing that “OCT may be a useful tool in evaluating the retinal circulation in diseases characterized by CNS involvement.”
Fernandes EA, Wildner P, Oset M, et al. Optical coherence tomography angiography as a potential tool in differential diagnosis of multiple sclerosis and rheumatic disorders with central nervous system involvement. Int Ophthalmol. 2024;44:281. 1. |


