 |
|
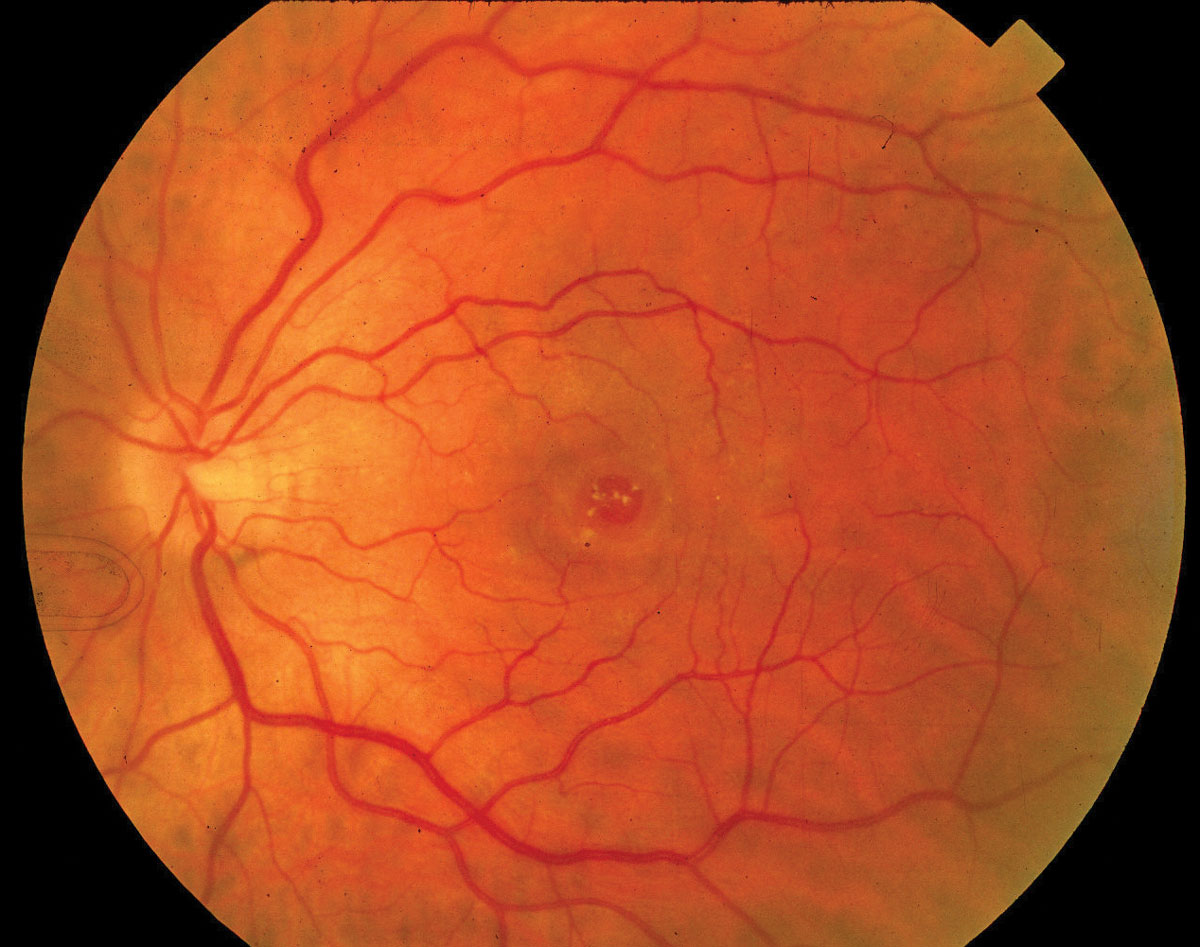
Though FDP may confer more benefits on patients with macular holes with minimum linear diameters ≥400µm, the findings of this study don’t support a linear treatment variation by macular hole size. The anatomic and visual effects in holes ≥500µm weren’t as certain. Photo: Diana Shechtman, OD. Click image to enlarge. |
Following a gas tamponade for macular hole repair, patients are often advised to undergo face-down positioning (FDP) in order to encourage apposition and healing. However, this practice is hotly debated among retinal surgeons and the guidelines for this practice aren’t consistent. Additionally, FDP is a significant burden to patients. Is this post-surgery posture really necessary for successful outcomes? Researchers investigated this question and reported in Ophthalmology that FDP may offer modest improvements in anatomical and visual outcomes.
The researchers conducted a prospectively registered systematic review and individual patient data meta-analysis of five randomized trials (n=379 eyes) that compared FDP to no FDP in adults who had undergone vitrectomy with gas tamponade for idiopathic full-thickness macular hole repair.
The researchers reported that the adjusted odds ratio for primary closure with FDP vs. no FDP was 2.41, which carries a relative risk of 1.08. The number needed to treat was 15—i.e., 15 patients would need to undergo FDP for three to 10 days in order for one of them to have an additional hole closure over no posturing, the researchers explained in their Ophthalmology paper. The FDP group had a mean improvement in postop visual acuity (-0.08 logMAR) vs. the no FDP group.
The researchers also noted in their paper that patients with larger holes of minimum linear diameter ≥400 µm had more certain benefits from FDP. The adjusted odds ratio for closure ranged from 1.13 to 10.12 and mean visual acuity improved between -0.18 to -0.01 logMAR. Each additional day of FDP was also associated with improved chances of anatomical success and improvement in vision. Thirteen days was considered the potential plateau for this benefit.
“Considering the generally safe and straightforward nature of this intervention, we recommend considering FDP for full-thickness macular holes larger than 400µm, with a minimum of three days posturing, pending further research,” the researchers concluded in their Ophthalmology paper. “Our confidence in these findings remains low-to-moderate, emphasizing the need for ongoing trials that could affect both our confidence and the estimates themselves.”
Raimondi R, Tzoumas N, Toh S, et al. Facedown positioning in macular hole surgery: a systematic review and individual participant data meta-analysis. Ophthalmology 2024. [Epub ahead of print]. |


