 |
|
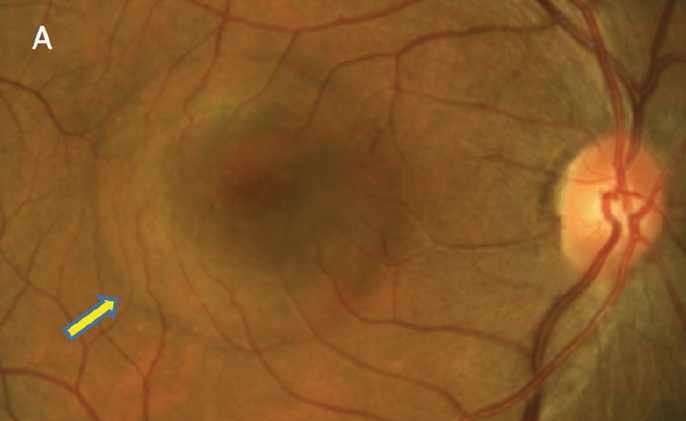
Sex and age are associated to the density of sex-steroid receptors in the human choroid tissue. Young women may derive protection against CSC through choroidal endothelial cells that are less responsive to female sex hormones. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
Dysfunction of the choroidal vasculature has been thought to be part of the underlying pathology in central serous chorioretinopathy (CSC), based on clinical manifestations diagnosed with multimodal imaging. There also might be a role for sex-steroid hormones (androgens, estrogens and progesterone) in the pathogenesis of CSC, due to its higher male prevalence and the fact that pregnancy-associated CSC normally resolves after childbirth.
Researchers in the Netherlands investigated the presence of sex-steroid receptors in human choroidal tissue across different ages and sexes, aiming to better understand the pronounced sex difference in the occurrence of the condition. They found that the number of sex-steroid receptors in the choroidal tissue differs between men and women across different ages, which aligns with the CSC prevalence patterns in men and postmenopausal women.
The study used enucleated eyes of 14 premenopausal women, 15 postmenopausal women, 10 young men (<45 years) and 10 older men (>60 years). Immunostaining was performed to detect the presence of androgen, progesterone and estrogen receptors. The stained slides were scored in a blinded manner for positive endothelial cells and stromal cells in consecutive sections of the same choroidal region.
The higher prevalence of CSC in men compared with women argues for androgens as a risk factor. The mean proportion of androgen receptor–positive endothelial cells was higher in young men (46%), compared with aged-matched women (29%). Premenopausal women showed markedly lower mean proportion of estrogen receptor (5%) and progesterone receptor endothelial cells (2%) compared with postmenopausal women (15% and 19%), young men (13% and 21%) and older men (18% and 27%). Mean progesterone receptor-positive stromal cells were also less present in premenopausal women (12%) than in other groups.
“Our data indicated differences in sex-steroid receptor expression between the sexes and age groups in choroidal endothelial cells but not in stromal cells,” the researchers wrote in their paper for Investigative Ophthalmology & Visual Science. “Therefore, endothelial cells are the candidate cell type in which differential expression of sex hormones may contribute to CSC disease risk.”
The team noted that the prevalence of CSC in women follows different patterns than in men, as CSC manifests more in older women and occasionally during pregnancy. Their finding that higher progesterone receptor expression in postmenopausal women compared with premenopausal women suggests that this may be a risk to CSC in women.
“To unravel the pathophysiologic mechanisms behind the striking difference in prevalence of CSC between men and women, further in vitro studies may focus on the effect of sex hormones (androgen or progesterone) on induced pluripotent stem cell-derived endothelial cells from patients with CSC—providing additional information on how sex hormones change endothelial cell functionality,” the study concluded.
Galuh S, Meijer OC, Brinks J, et al. Differential expression of sex-steroid receptors in the choroid aligns with central serous chorioretinopathy sex prevalence across different ages. Invest Ophthlamol Vis Sci. 2024;65(8):5. |


