 |
|
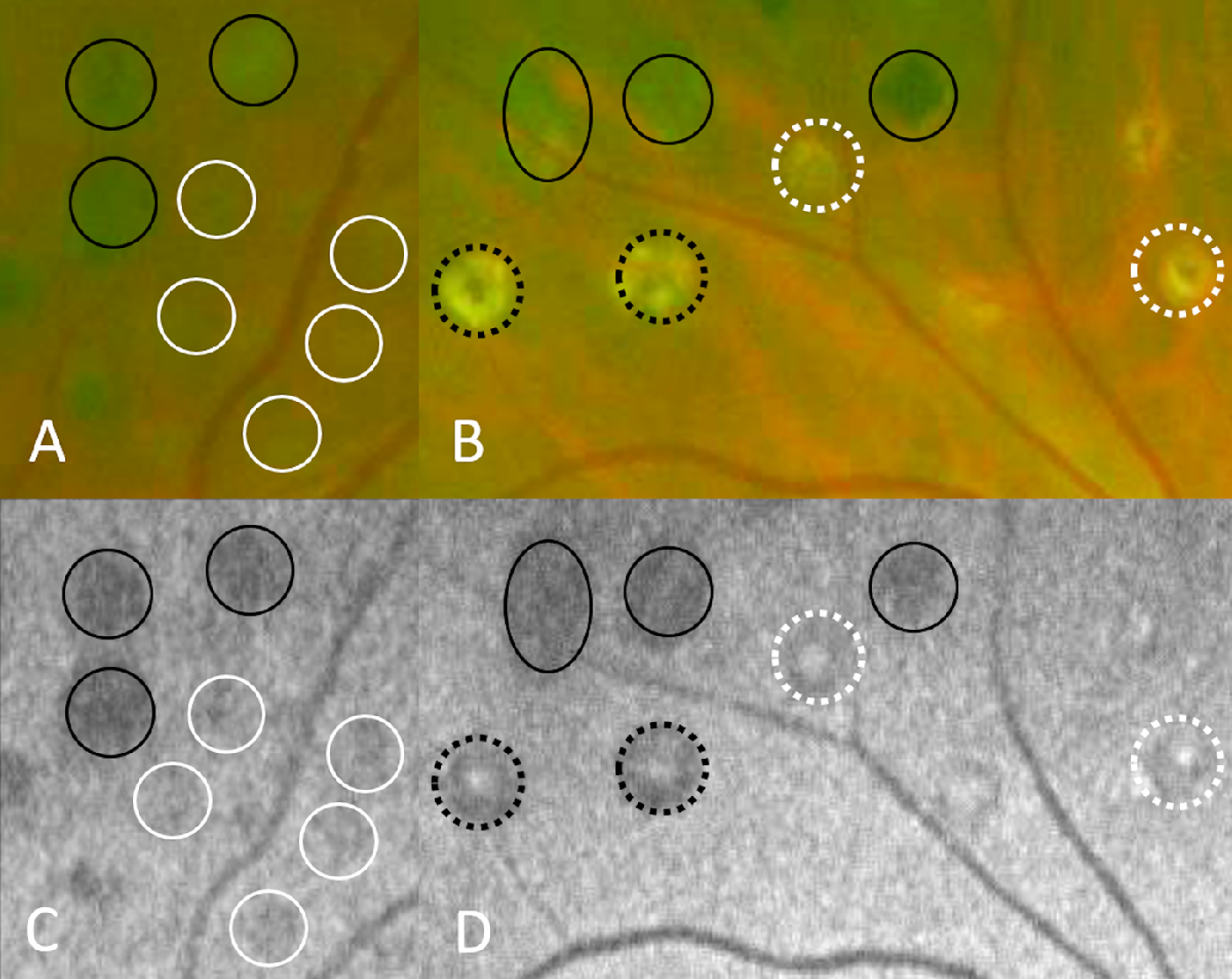
This image from the study shows areas of photocoagulation on fundus photography (A, B) and autofluorescence (C, D). The researchers correlated these areas with microperimetry results and demonstrated some preservation of photoreceptor function. (Black circle: no FAF signal; white circle: lesions with diffuse FAF; white-dotted circle: lesions with white-dotted centers and diffuse FAF in the background; black-dotted circle: lesions with white-dotted centers and no background FAF.) Photo: Nishida K, et al. Transl Vis Sci Technol. 2024;13(7):1. Click image to enlarge. |
Given that fundus autofluorescence (FAF) enables observation of RPE cells, a new study sought to determine whether this imaging method could be used to estimate damage to photoreceptors after panretinal photocoagulation (PRP) in patients with proliferative diabetic retinopathy (PDR), which could help determine the need for additional treatment.
In the retrospective cohort study, the researchers evaluated the relationships among morphology, FAF and retinal sensitivity of photocoagulated lesions more than one year after PRP in 19 patients (11 male; average age, 62.5) with PDR and good vision. Lesions were classified according to FAF levels:
- group A, no FAF (n=37);
- group B, diffuse FAF (n=39);
- group C, white-dotted centers with diffuse FAF (n=4);
- group D, white-dotted centers without FAF (n=15); and
- group E, controls (n=39).
The table below displays the average findings from each group:
Group | Number of Lesions | Median Sensitivity (dB) | Ellipsoid Zone (EZ) Lines Absent (%) | Inner Retinal Layer Damage (%) |
A | 37 | 0.0 | 93.5 | 45.2 |
B | 39 | 18.0 | 18.1 | 3.0 |
C | 4 | 13.9 | 50.0 | 50.0 |
D | 15 | 0.3 | 93.3 | 73.3 |
E | 39 | 21.5 | 0.0 | 0.0 |
“The present study revealed that photoreceptors in most photocoagulated lesions with diffuse FAF retained some retinal sensitivity and the morphology of the EZ line and inner retinal layer more than one year after PRP for PDR,” the researchers explained in their paper on the study, published in Translational Vision Science & Technology. They also noted that, to their knowledge, “this study is the first to suggest that some photoreceptors are preserved and functional in most photocoagulated lesions with diffuse FAF.”
The researchers offered one hypothesis in their paper regarding the mechanism underlying the efficacy of PRP for PDR, being that “it decreases the number of photoreceptors consuming a large amount of oxygen in the outer retina and improves hypoxia in the inner retina by inducing oxygen transport from the choriocapillaris. However,” they continued, “photocoagulated lesions with diffuse FAF seem to have photoreceptors from this study, and photocoagulated lesions with diffuse FAF after PRP may be less effective at the aspect of photoreceptor destruction. FAF of photocoagulated lesions after PRP can indicate the preservation of photoreceptor noninvasively; thus, they can help to determine the need for additional PRP for the severe ischemic diseases, such as refractory neovascular glaucoma cases.”
This study has several limitations in addition to its small sample size, such as its retrospective design, which made it impossible to evaluate the burn strength immediately after laser delivery. The findings could be validated in the future through a prospective study.
“In conclusion,” the researchers wrote in their paper, “the study findings suggest that photoreceptors in most photocoagulated lesions with diffuse autofluorescence retain their morphology and function. Using FAF, the damage to photoreceptors after PRP can be estimated in a noninvasive manner in patients with diabetes; this process can help to determine the need for additional PRP.”
Nishida K, Kawasaki R, Fukushima Y, Takahashi S, Fujikado T, Nishida K. Morphology, fundus autofluorescence, and retinal sensitivity of photocoagulated lesions in proliferative diabetic retinopathy. Transl Vis Sci Technol. 2024;13(7):1. |


