 |
|
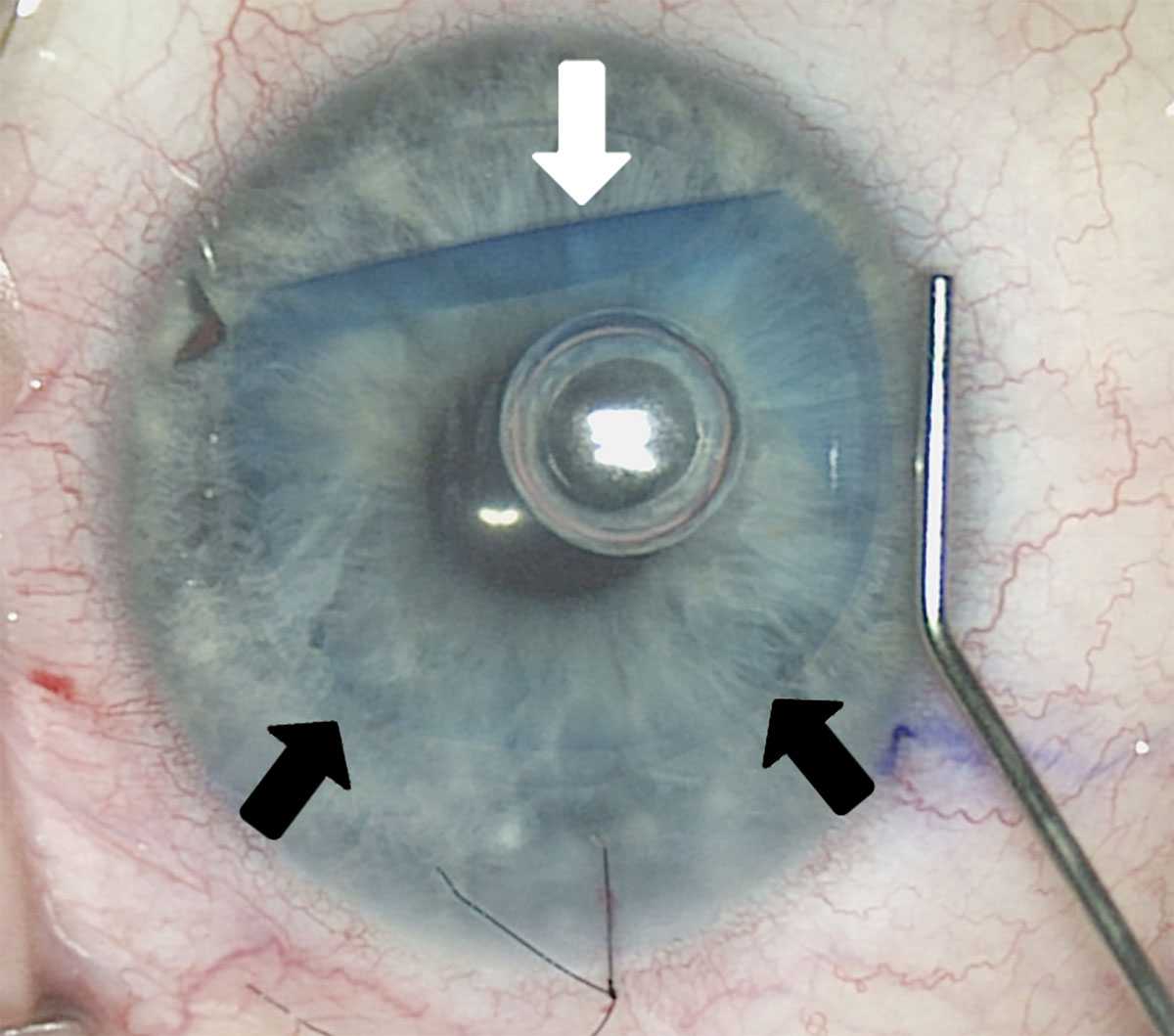
Visual outcomes were comparable for eyes undergoing repeat DMEK for technical failure with controls but were worse for those undergoing the procedure for secondary graft failure. This may be due to a longer duration of corneal edema in these eyes, which would also partially explain higher rates of post-op anterior backscattering when compared with the technical failure eyes. Photo: Kathleen Kelley, OD, Francis Price, Jr., MD, and Marianne Price, PhD. Click image to enlarge. |
A partial-thickness corneal transplant procedure is a great option for certain subsets of patients, especially those with corneal endothelial disorders. In particular, the operation of Descemet’s membrane endothelial keratoplasty (DMEK) was recently evaluated by researchers in repeated instances for technical failure and secondary graft failure.
The retrospective Cornea study included a total of 49 eyes that underwent repeat DMEK for technical failure (persistent graft detachment, n=24) or secondary graft failure (late endothelial graft failure, n=25). Both Fuchs’ endothelial corneal dystrophy (80%) and bullous keratopathy (20%) were surgical indications for DMEK. Outcome measures included best-corrected visual acuity (BCVA), endothelial cell count, corneal backscattering, pachymetry and graft survival. Outcomes were also compared with 49 age-matched controls with primary DMEK eyes.
LogMAR BCVA improved from 0.92 ±0.6 before to 0.20 ±0.3 at one year after repeat DMEK, seeing better outcomes in the technical failure cases than in eyes with secondary graft failure. Donor endothelial cell count decreased, from 2,618 ±171cells/mm2 at baseline to 1,247 ±422cells/mm2 after one year; no differences were seen in endothelial cell count between technical failure and secondary graft failure eyes. However, one-year BCVA and endothelial cell counts were both better in the control group than the repeat DMEK group. Graft survival probability of five years after repeat DMEK was better for eyes with technical failure (100%) than for those with secondary graft failure (75%). Graft survival of this time frame was also better in patients with Fuchs endothelial cell dystrophy (95%) than bullous keratopathy (65%) as a primary indication for surgery.
|
For an overview of lamellar corneal surgeries, see this recent feature. |
In their discussion section, the study authors relay that the five-year survival probability after repeat DMEK is comparable to the survival rate after primary DMEK, with rates of 87% and 90%, respectively. This is somewhat incongruous with the dissimilar rates of survival seen in the current study of secondary graft failure eyes (75%) vs. technical failure eyes (100%), suggesting that graft survival may depend on preexisting pathology of the host. One previous report found elevated cytokine levels linked with amplified innate immune response present in the aqueous humor of eyes with endothelial graft failure; this factor may contribute to differences in survival probabilities seen between the groups studied in this investigation.
What’s more, the similar rates of graft detachment seen in this study after repeat DMEK between the technical and secondary graft failure groups may suggest prior graft detachment is not actually a predetermining factor after repeat DMEK; otherwise, a higher rate of detachment would be expected in eyes with technical failure.
The authors make note of an unusually high drop in endothelial cell density in about half of eyes with secondary graft failure, which occurred about two years before a confirmed diagnosis. They argue that “this parameter could serve as a promising indicator to recognize eyes at risk of late endothelial graft failure, suggesting the necessity for more vigilant monitoring in such cases.”
Laouani A, Vasiliauskaite I, Bourgonje VJA, et al. Clinical outcomes of repeat Descemet membrane endothelial keratoplasty after graft failure. Cornea. 2024;00:1-8. |


