 |
|
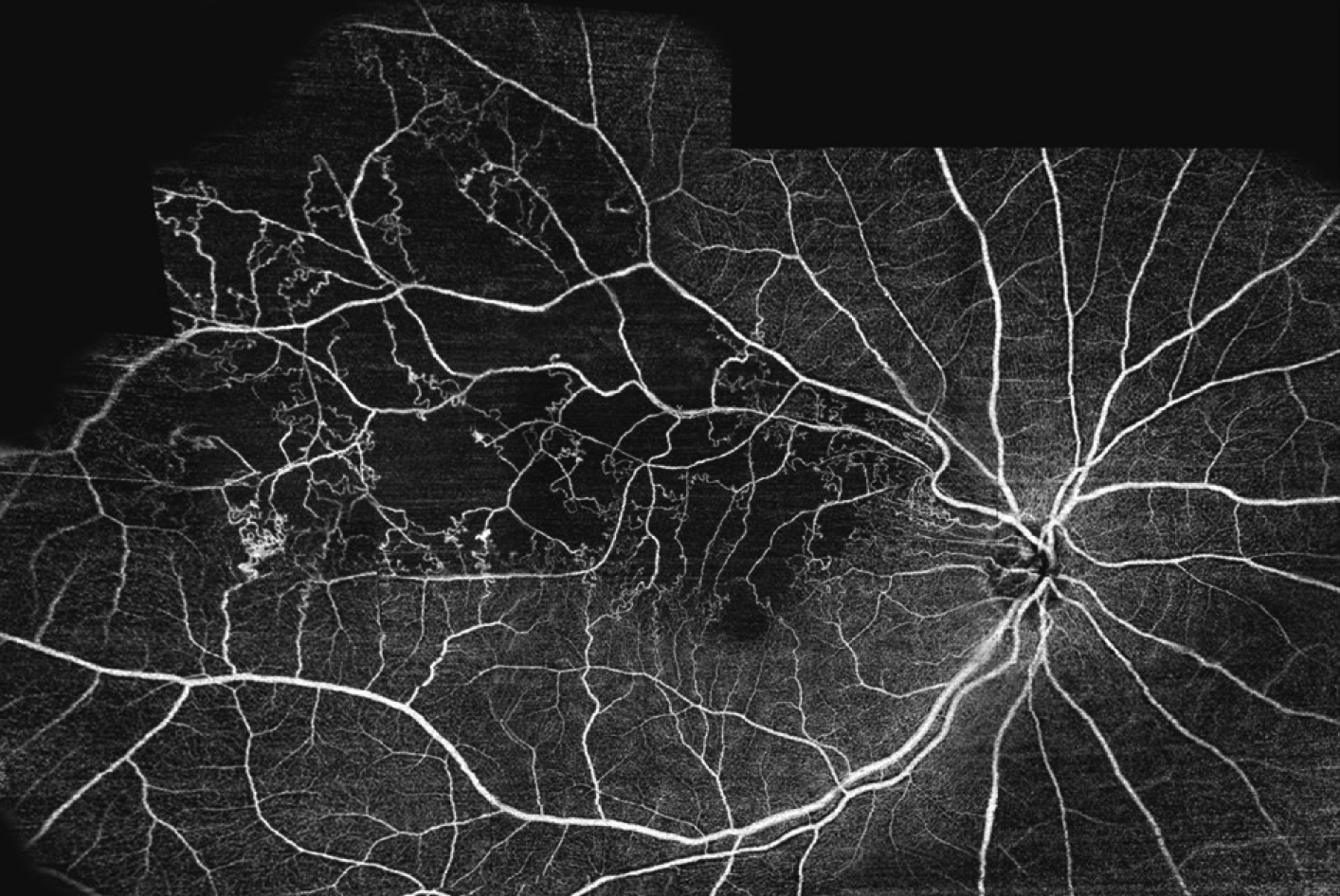
A new study published in the journal Eye quantifies the substantial incidence of a glaucoma diagnosis in patients who previously experienced a retinal vein occlusion. Researchers found that screening tests to confirm open-angle glaucoma were often performed well after the initial RVO diagnosis, or not performed at all, illuminating the risks involved with this delay in care including retinal nerve fiber layer thinning and visual field loss. Photo: Topcon. Click image to enlarge. |
The causal relationship between glaucoma and the development of retinal vein occlusions has been well recognized; however, mounting evidence supports a reciprocal relationship between the two diseases. A new cross-sectional study spanning 30 years found that patients diagnosed with central retinal vein occlusion (RVO) were at a greater risk of developing open-angle glaucoma (OAG). Most concerning to researchers was the amount of time in between the initial vein occlusion and the glaucoma diagnosis, underscoring the urgency for timely diagnosis and management.
Published in the journal Eye, the study included patients diagnosed with OAG after RVO who were then matched 2:1 with RVO patients without prior glaucoma. Of 1,178 RVO patients without initial OAG, 4.5% were later diagnosed with glaucoma after an average of 5.5 ±6.1 years. These patients were also more likely to have been diagnosed with central retinal vein occlusion rather than branch retinal vein occlusion.
According to the study, screening tests for OAG were performed at a higher frequency in those who were diagnosed with the disease compared to those who never received one. Specifically, visual fields testing was conducted in 21.6% of OAG-diagnosed patients vs. 10.8% of those without an OAG diagnosis, while retinal nerve fiber layer (RNFL) imaging was performed in 52.9% of OAG-diagnosed patients compared to 27.4% of those without OAG. The mean deviation of VF was significantly lower in eyes with a history of RVO compared with the fellow unaffected eyes. Predictive factors for OAG diagnosis included elevated intraocular pressure and cup-to-disc ratio in the fellow eye, as well as the absence of macular edema in the RVO-affected eye.
“The extent of VF loss and RNFL thinning in the fellow eye at the time of OAG diagnosis underscores the urgency for timely detection and intervention,” the researchers wrote in their paper. “This inference is further supported by the fact that screening tests, typically employed to confirm OAG, were often performed well after the initial RVO diagnosis, or sometimes not performed at all.”
The authors pointed out the ways in which the patients in this study differed from the typical glaucoma diagnosis, which usually affects both eyes. “In our study, patients subsequently diagnosed with OAG rarely had the condition exclusively in the eye affected by an RVO,” they wrote. “This suggests that the risk of developing OAG is related to patient-level factors rather than factors specific to having an RVO, such as fluctuations in IOP, damage to the RNFL, or the presence of hemorrhages.” The lower rate of visual field testing vs. RNFL scans in RVO patients “could be due to concerns about reduced visual acuity, age-related limitations, or potential impacts of retinal hemorrhages, ischemia, or laser treatment on the accuracy of VF results.”
Other interesting findings noted in the study included the realization that patients diagnosed with glaucoma were more likely to require panretinal laser photocoagulation, potentially revealing increased complications from RVO due to retinal ischemia and subsequent neovascularization and hemorrhaging. Researchers were also surprised that these patients were less likely to have macular edema, “despite being equally likely to receive intravitreal injections of steroids or agents targeting vascular endothelial growth factor,” they wrote. “This finding could be partly attributed to changes in the availability and types of RVO treatments during our study.”
Coding variability and reliance on electronic medical records may have affected the precision of glaucoma diagnoses in this study, the authors pointed out. “However, a strength of our study is our detailed review of each chart, including scanned records, to identify when OAG was initially diagnosed,” they noted in their paper. “Comparing ICD-10 codes with an analysis of each chart also enhanced the clinical classification accuracy.” They also noted the potential for selection bias toward patients with more severe disease, considering the study was conducted at a retina and glaucoma referral center. “Finally, our study population, comprised of well-insured, suburban patients from an academic medical center, lacked racial and ethnic diversity,” wrote the authors. “Future research should address these gaps, as racial and ethnic minority groups often bear a disproportionate burden of RVOs and OAG and encounter challenges in accessing eye care and obtaining accurate diagnoses.”
The authors concluded by strongly advocating for the implementation of screening tests for glaucoma as part of the standard of care for patients with retinal vein occlusions. “Given the evidence presented on delayed screening tests and the potential contribution of unmanaged OAG on RNFL thinning and VF loss, proactive measures are imperative in addressing this pressing concern in patient care,” they said. “Adopting this approach can lead to earlier disease detection and improved outcomes for patients affected by both sight-threatening conditions.”
Muhtaseb RE, Huther A, Alwreikat AM, et al. Optimizing open-angle glaucoma risk assessment in patients with retinal vein occlusions. Eye. July 9, 2024. [Epub ahead of print.] |


