The AREDS1 and AREDS2 multicenter randomized placebo-controlled trials showed salutary effects in slowing of age-related macular degeneration (AMD) to advanced stages of the disease. However, specific trends in geographic atrophy (GA) progression during the trials were not teased out in the original analysis. In light of the increased emphasis on GA therapy now that two injectable drugs have been approved, the AREDS investigators went back to their data for another look.
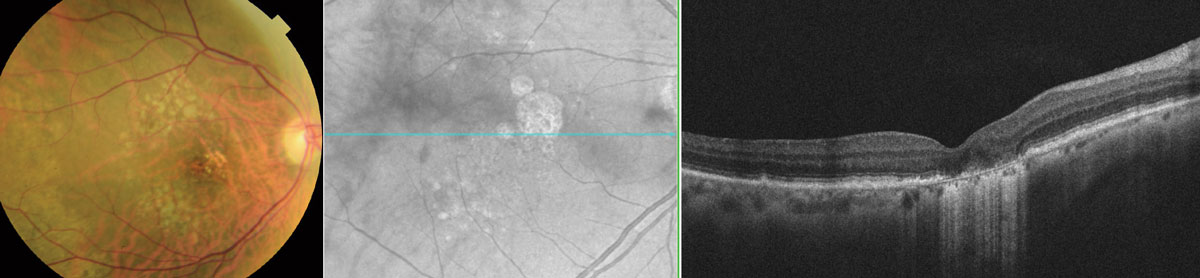 |
| This analysis suggests that patients with non-central geographic atrophy in one or both eyes may derive the most benefit from supplementation that includes vitamins C and E, and lutein/zeaxanthin, but not β-carotene, according to the study authors’ report in the journal Ophthalmology. Photo: Wendy Harrison, OD, PhD. Click image to enlarge. |
AREDS1 participants were randomly assigned to receive oral antioxidants (vitamins C and E plus β-carotene), zinc, a combination of these or placebo, while individuals in the AREDS2 study were randomized to lutein/zeaxanthin, docosahexaenoic acid/eicosapentaenoic acid, combination or placebo.
The main outcomes measures of this new post hoc analysis of those trials were measures of GA growth toward the fovea and overall lesion size. The study included 392 eyes and 1,210 eyes with geographic atrophy from the AREDS1 and AREDS2 multicenter randomized placebo-controlled trials, respectively.
The study—published on Tuesday in the journal Ophthalmology—suggests that oral antioxidant supplementation comprised of high daily doses of vitamin C, vitamin E and β-carotene (AREDS1) slows progression of GA towards the central macula by about 36% (50.7μm/year vs. 72.9μm/year). Similarly, oral lutein/zeaxanthin supplementation in AREDS2 eyes not receiving β-carotene led to a comparable slowing of progression toward the macula, this time by about 36% (80.1μm/year vs. 114.4μm/year), the study authors reported in their Ophthalmology paper.
Treatment effects on overall lesion size were more complex. The data showed no significant difference in area-based progression in either the AREDS1 or AREDS2 datasets of eyes with any GA, be it central or non-central. However, growth was significantly slower in eyes of participants randomized to β-carotene than no β-carotene (0.264mm/year vs. 0.301mm/year).
“The likely unifying explanation for differences in proximity-based vs. area-based progression, and for eyes with central vs. non-central GA, is efficacy in slowing GA progression predominantly in the central and paracentral macula, as opposed to the peripheral macula,” the authors wrote, which would account for the foveal proximity improvements noted. Since the central ETDRS subfield accounts for just 3% of the full macular grid, any disease-sparing effects here would only constitute a very small proportion of the whole macular area and thus minimal efficacy would be observed in measures of total area. “However, area-based efficacy would be detected preferentially in eyes with non-central GA,” they added, “where GA area is small, such that decreased progression into the central/paracentral macula would also affect the GA area metric.”
The authors go on to explain that lutein and zeaxanthin “are highly abundant in the very central macula (i.e., the central ETDRS subfield),” with lower abundance paracentrally and the lowest beyond that point.” Hence, their known distribution appears consistent with the preferential efficacy of supplementation in slowing proximity-based progression in non-central GA. This agreement provides strong biological plausibility for the pattern of results.”
These findings have important implications for the potential preservation of visual function in the long term, the study authors argue. “These results also highlight important differences in mechanisms of geographic atrophy progression in the central vs. peripheral macula and have implications for our understanding of the mechanisms of foveal sparing.”
While commenting on the impact of their work, the researchers noted in their paper that this research “may justify a prospective randomized controlled trial of oral antioxidant and lutein/zeaxanthin supplementation in eyes of individuals with non-central GA. If the results were confirmed, this would suggest a new standard of care for patients with geographic atrophy.”
Overall, in the AREDS population of eyes with non-central GA, the prevalent cohort demonstrated a treatment effect with antioxidants for proximity-based but not area-based GA progression, while the incident cohort demonstrated the opposite.
Keenan TDL, Agrón E, Keane PA, et al. Oral Antioxidant and Lutein/Zeaxanthin Supplements Slow Geographic Atrophy Progression to the Fovea in Age-Related Macular Degeneration. Ophthalmology. July 16, 2024 [Epub ahead of print]. |


