 |
|
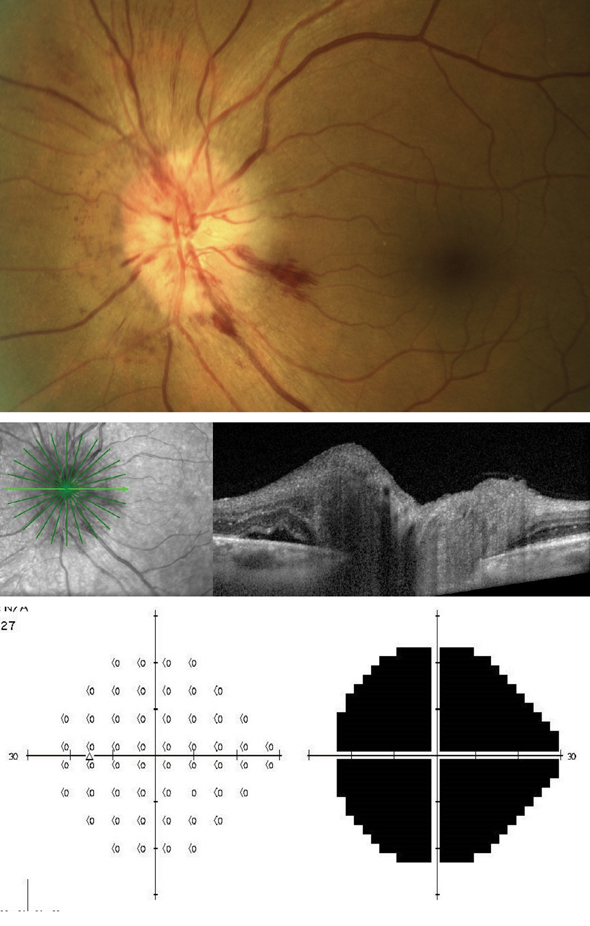
Researchers in this study note that accurately identifying suspected AAION in patients is critical, as untreated giant cell arteritis can carry a high risk of bilateral involvement. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
Identifying whether anterior ischemic optic neuropathy is arteritic (AAION) or non-arteritic (NAAION) can make an already stressful patient encounter all the more nerve-wracking. One new study has sought to lower the stakes for doctors by identifying characteristics that distinguish the two from each other. The researchers were able to identify clinical, biological and ophthalmological variables indicative of either one of the conditions.
As one of the largest studies examining this question, it included 94 AAION and 94 NAAION patients. The retrospective analysis compared clinical, biological and ophthalmologic characteristics at baseline in both sets of patients.
Researchers found that arteritic patients included had a higher likelihood of displaying arterial hypertension as well as being older in age. As well, cephalic symptoms and acute-phase reactants were more frequent in this group at baseline, as were profound vision loss, bilateral involvement and delayed choroidal perfusion. Only observed in arteritic patients were central retinal and cilioretinal occlusions.
After analyzing the trends, researchers independently associated a diagnosis of AAION with the characteristics of an age greater that 70 years, an absence of splinter hemorrhage, delayed choroidal perfusion, CRP level and platelet count.
Despite the higher frequency of delayed choroidal perfusion seen in arteritic cases, the researchers point out that this is not pathognomonic for AAION, since about 20% of non-arteritic patients also experience this. Additionally, the cupping sign of acquired excavation of the optic nerve head that suggests AAION is limited in its relevance to the emergency setting, as it appears at a late stage.
Related to their evaluation of platelet count, the researchers mention a prior study that corroborates their findings, reporting giant cell arteritis (GCA)–related AION expressed significantly higher platelet counts, ESR and CRP levels. The high platelet count and CRP level combined increased the likelihood of developing GCA in those with AION.
The researchers make sure to mention this as well, explaining that accurately identifying suspected AAION in patients is critical, as untreated GCA can carry a high risk of bilateral involvement. Fortunately, this is a very manageable issue, typically preventable with high-dosage glucocorticoids. They do note, though, that this treatment can be detrimental to elderly patients with NAAION, making the research’s aim of characteristic expression even more palpable in importance.
Echoing this sentiment, the authors state that “overall, distinguishing AAION and NAAION is a challenge in daily practice, but is crucial because the two conditions require a different approach in terms of work-up and treatment.” As for what their research adds to clinical practice, the believe “this model can help to discriminate of AAION and NAAION, thus ensuring prompt and appropriate treatments for both patient populations.”
Parreau S, Dentel A, Mhenni R, et al. Clinical, biological, and ophthalmological characteristics differentiating arteritic from non-arteritic anterior ischemic optic neuropathy. Roy Col Ophthalmol. October 22, 2022. [Epub ahead of print]. |


