 |
| A new artificial intelligence-based grading scale may be suitable for widespread application in the screening of pathologic myopia, its developers argue. Photo: Kengo Hayashi, MD. Click image to enlarge. |
Pathologic myopia is a leading cause of irreversible blindness and projected to affect 55 million people globally by 2050, underscoring the need for new research and instruments to advance diagnosis and progression monitoring. Recently, a group of doctors in Beijing developed a novel tool to grade diffuse chorioretinal atrophy (DCA) in these patients using a modern technology that has gradually been making its way into eye care: artificial intelligence. The new classification system categorizes DCA into three groups—G1, G2 and G3—based on the area and density of diffuse atrophy. High myopes without diffuse atrophy were designated as G0. See the chart below for a breakdown of the clinical criteria for each grade.
Table 1. Proposed classification of diffuse chorioretinal atrophy
Area (mm2) | Density | Clinical defining features | |
Grade 0 | 0 | 0 | No diffuse chorioretinal atrophy lesions; or lesions were not identified by artificial intelligence |
Grade 1 | 0 < area ≤ 10.170786 | 0.000 < density ≤ 0.093 | The atrophic lesions were located in the temporal region of the optic disc, exhibiting indistinct boundaries and a punctate distribution pattern. The fovea within the macular area remained unaffected by these lesions. Within these areas of atrophy, choroidal vascular structures appeared significantly blurred or absent, often displaying perivascular circumferential involvement |
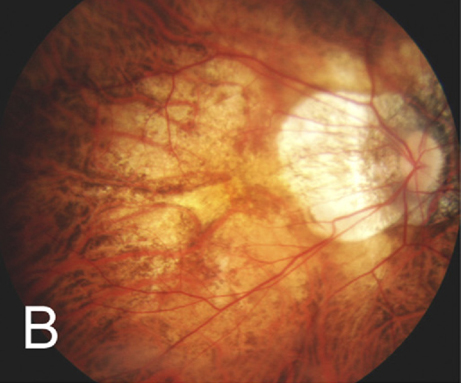
Grade 2 | 10.170786 < area ≤ 27.034940 | 0.093 < density ≤ 0.245 | The atrophic lesions exhibited large yellow-white sheets with indistinct margins, frequently localized around the optic disc, and involved the fovea. However, these lesions generally did not extend beyond the temporal aspect of the macula. Choroidal vascular structure was disrupted or absent within the atrophic lesions |
Grade 3 | 27.034940 < area ≤ 77.894083 | 0.245 < density ≤ 0.712 | The yellowish-white atrophy lesions exhibit indistinct borders and are widely distributed throughout the eye. Within the atrophic areas, the choroidal blood vessel structure completely vanishes |
The team tested the grading scale on a group of 202 patients (338 eyes) who underwent comprehensive examinations. They explained in their paper on the study, published this week in Ophthalmology and Therapy, that “the methodology involved image preprocessing, sample labeling, employing deep learning segmentation models, measuring and calculating the area and density of DCA lesions.” Once the data were obtained, statistical analysis was used to grade lesion severity of DCA, and grades (G0 to G3) were assigned to describe the morphology of corresponding fundus photos.
The fundus photographs “depicted a progressive enlargement of atrophic lesions, evolving from punctate-shaped to patchy with indistinct boundaries,” the study authors wrote in their paper. “DCA atrophy lesions exhibited a gradual shift in color from brown-yellow to yellow-white, originating from the temporal side of the optic disc and extending towards the macula, with severe cases exhibiting widespread distribution throughout the posterior pole.”
Compared to patients without DCA, those with this finding were older (34 vs. 29 years), had a longer axial length (28.6mm vs. 27.1mm) and exhibited a more myopic spherical equivalent (-13.00 vs. - 9.09). The authors pointed out, “In eyes with DCA, a trend emerged as grades increased from G1 to G3, showing associations with older age, longer axial length, deeper myopic spherical equivalent, larger area of parapapillary atrophy and increased fundus tessellated density.”
The results of this study suggest this new AI grading scale is an effective method of classifying DCA and severity based on area and density and may be suitable for widespread application in pathologic myopia screening, the authors proposed. “Early detection, diagnosis and treatment are crucial in reducing the incidence of myopia-related blindness and implementing timely interventions for pathologic myopia,” they concluded.
Niu YN, He HL, Chen XY, et al. A novel grading system for diffuse chorioretinal atrophy in pathologic myopia. Ophthalmol Ther. March 5, 2024. [Epub ahead of print]. |


