 |
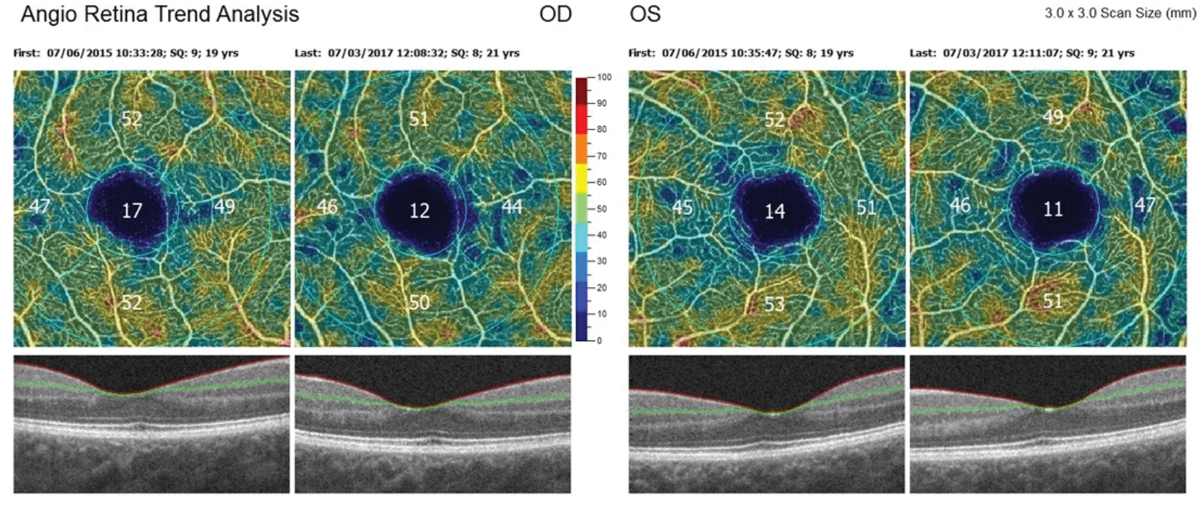
| The retina acts as a projection of the central nervous system, providing a more convenient and accessible way to detect certain brain disorders. New research ties retinal vascular changes in diabetes (such as this case’s decline in vessel density over time) to cerebral small-vessel disease. Photo: Steven Ferrucci, OD. Click image to enlarge. |
While diabetes complications like retinopathy and macular edema have become routine to check and manage within the eyecare community, other complications of the disease have not. Specifically, diabetic encephalopathy (DE) results in cognitive impairment ranging from mild forms to dementia but this manifestation has no gold standard for diagnosis, mainly relying on clinical neuropsychological scale evaluation and diabetic cerebral small-vessel disease (CSVD)-related MRI findings.
New research used the capabilities of OCT angiography (OCT-A) to evaluate retinal vascular density in diabetic CSVD, as well as map the relationship between retinal VD and cerebral MRI markers and cognitive function. Doing so, the researchers hoped to elucidate if OCT-A could be used as a tool for early CSVD diagnosis.
Enrolled in the study were 131 total patients; the CSVD group made up 43 individuals and 88 comprised the non-CSVD group. MRIs performed on patients revealed that the most common marker in the diabetic CSVD group was white matter hyperintensities (WMHs), particularly deep WMHs (58.8%), followed by cerebral microbleeds in the subtentorial and cortical areas (34.8%). Increased prevalence of cognitive dysfunction and depression, along with decreased visuospatial and executive ability and delayed recall ability were all observed in the CSVD group.
Turning to the OCT-A results vessel densities of the macular superficial vascular plexus, intermediate capillary plexus and deep capillary plexus were all lower in the CSVD group than those in the non-CSVD group. Analysis revealed that macular superficial vascular plexus vessel density was independently associated with cerebral microbleeds and macular intermediate capillary plexus density was associated with white matter lacunar infarcts. From these results, the study authors relay that OCT-A could be a highly valuable and practical technique for screening or diagnosing diabetic CSVD.
In an article for Diabetes, Obesity and Metabolism, the researchers elaborate on their findings, confirming that deep WMHs were both typical and predominant as a diabetic CSVD marker and was associated with cognitive dysfunction. Almost half of CSVD patients had cerebral microbleeds or perivascular spaces, and the next most common marker was lacunar infarction. Cerebral microbleeds have been revealed in recent research to be responsible for cognitive impairment development in diabetic patients, with the progression of vascular cognitive impairment being potentially accelerated with an increase in microbleeds. However, it was also found that hypertension aggravated severity of deep WMHs but not cerebral microbleeds.
It is not just cognitive dysfunction that should be paid attention to, though, as emotional disorders like depression and anxiety can also be manifestations of DE. Since depression prevalence was elevated in the diabetic CSVD patients of this study, mental health should be a concern in this population. Other CSVD risk factors are age, hypertension, diabetes and sex, but all are still controversial.
The authors emphasize that “screening and diagnosis of DE is still difficult and time-consuming, and there is a strong and urgent need to explore a convenient and practical method for screening and diagnosing DE.” As this study shows, the eye may be this ideal window to investigate brain disorders, including CSVD.
Huang Y, Wang S, Cai C, et al. Retinal vascular density as a potential biomarker of diabetic cerebral small vessel disease. Front Neurosci. February 26, 2024. [Epub ahead of print]. |


