The higher incidence of diabetic retinopathy and likelihood of developing diabetic macular edema (DME) in men compared to women has been established in the literature, and many believe inflammation plays a role in disease progression. A new study published in Ophthalmology Science used OCT to identify variations in these characteristics between both men and women with DME and found the male sex was associated with more inflammation-related biomarkers.
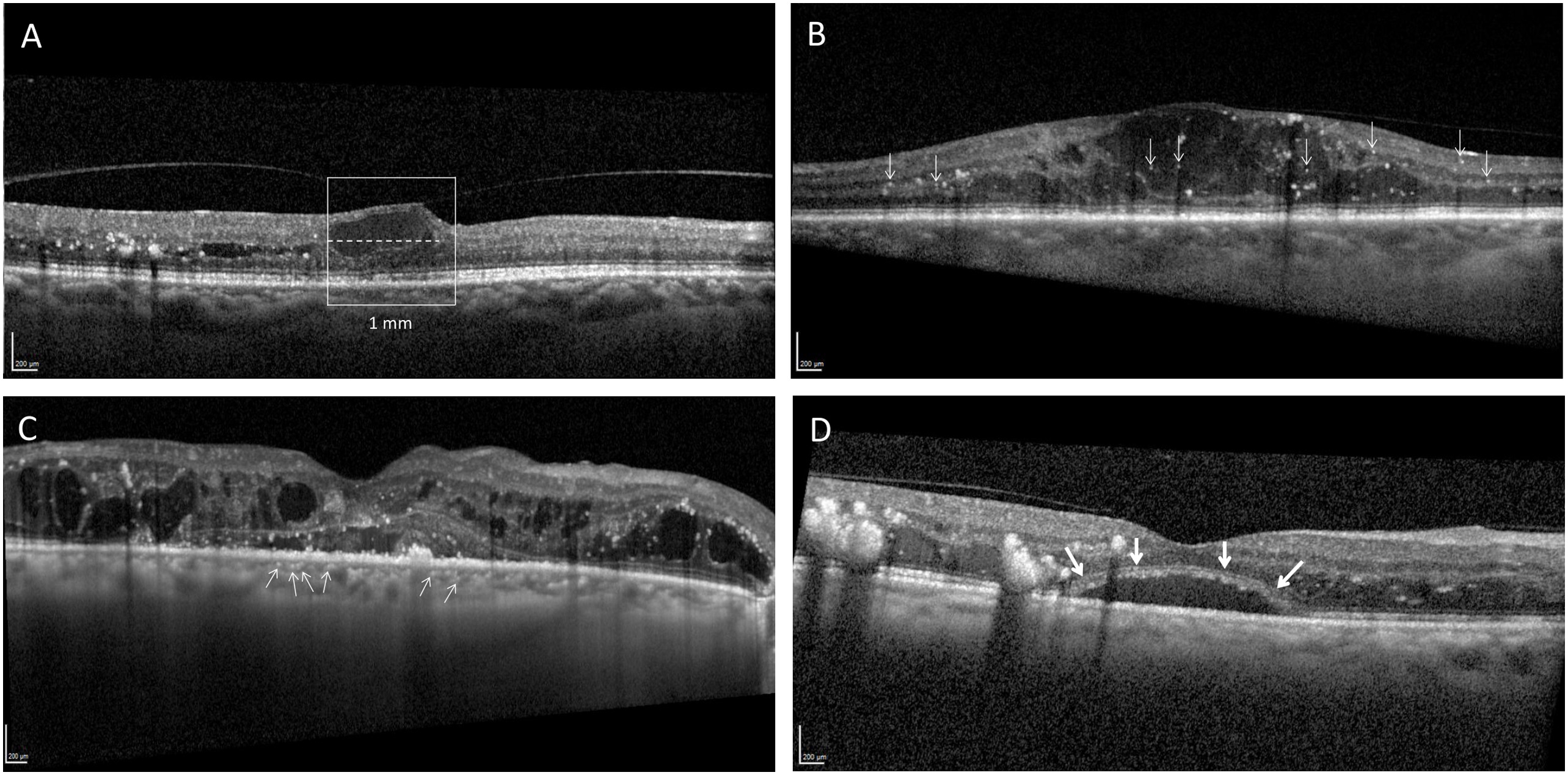 |
| Researchers suggest that male DME patients may require greater vigilance than women, owning to their more inflammatory response to the condition. This image from the study shows several inflammation-related biomarkers with differential findings for men vs. women: (A) disorganization of retinal inner layers (B) retinal hyperreflective foci, (C) hyperreflective choroidal foci and (D) subfoveal neuroretinal detachment. Photo: Chen X, et al. Ophthalmol Sci. July 18, 2024. Click image to enlarge. |
Conducted at the Zuckerberg San Francisco General Hospital, the retrospective study included 180 men and 106 women with DME who hadn’t received an anti-VEGF injection within the last six months, and researchers performed multivariate regression analyses to control for age, HbA1c levels and central macular thickness. Men had more retinal hyperreflective foci (HRF) (incidence rate 1.19), more hyperreflective choroidal foci (HCF) (1.2 vs. 0.8) and thicker inner nuclear layer (INL) in the pericentral area (44.6μm vs. 40.7μm). Female patients were found to have a larger extent of disorganization of retinal inner layers (493.5μm in male vs. 588.7μm in female). No significant difference between men and women was found for retinal nerve fiber layer or ganglion cell layer thickness.
In their paper, authors wrote that HRF is noticeably reduced following anti-VEGF treatment, but an even more significant reduction follows a dexamethasone intravitreal implant, meaning a patient with more HRF at baseline would have more reduction in macular edema and greater improvement in retinal sensitivity after dexamethasone treatment. This led to their hypothesis that “compared to female DME patients, male patients [who] had more HRF suggests increased microglial accumulation and activity in males even with similar control of blood glucose and similar amount of DME. It is possible that due to increased HRF at presentation, male patients could be on average more responsive to corticosteroid treatment, although more studies are needed to confirm this potential therapeutic implication.”
Men in the study also had more HCF when controlled for glycemic levels and the amount of DME, bringing in the matter of microglial cells, which are only found in the inner retina in healthy patients without diabetes. However, as inflammation persists, microglial cells spread posteriorly, creating more HRF in the outer retinal layers in patients with more severe diabetic retinopathy (DR). “The majority of eyes in our study with HCF also had HRF, supporting the hypothesis that HCF and HRF are on a spectrum,” said the authors. The increased hyperreflective foci in the retina and choroid seen in male DME patients implies increased microglial migration, the researchers wrote, likely due to inflammatory mediators and the breakdown of the external limiting membrane.
As for the biological reasoning behind these differences, sex hormones may be implicated. The authors mention the effect estrogen may have on reducing retinal vessel resistance and how it can protect against the impairment of blood flow in ocular diseases. Although many women in this specific study were post-menopausal, other research has found accumulated exposure to estrogen over the lifetime from menarche to menopause offers protective effects for ocular vascular diseases, noted the authors, who say that is in contrast to testosterone levels which are associated with the development and progression of DR.
The retrospective nature of this study made it impossible to control for all confounders, the authors said, most notably the overall severity of DR and duration of systemic diabetes.
The results of this study suggest that men may potentially require closer follow-ups, concluded the authors. “As HRF and HCF on baseline OCT were correlated with improved responsiveness to corticosteroid treatment in prior studies, there might be a role for a lower threshold for other treatment failures in men to switch to steroid injections for DME, especially when inflammation-related biomarkers are observed on OCT,” they said. “Future studies are needed to evaluate the potential implications of these sex-based differences of inflammation-related biomarkers on clinical outcomes and on tailored treatment.”
Chen X, Yang W, Fong A, Chahal N, Taha AT, Keenan JD, Stewart JM. Sex differences in inflammation-related biomarkers detected with Optical Coherence Tomography in patients with diabetic macular edema. Ophthalmology Science. July 18, 2024. [Epub ahead of print.] |


