 |
| Understanding the complex relationships among myopia severity, structural changes and functional changes can give clinicians a higher index of suspicion for glaucoma in affected individuals. Photo: Jarett Mazzarella, OD, and Justin Cole, OD. Click image to enlarge. |
Myopia has shown a significant association with increased primary open-angle glaucoma rates, particularly in patients with high refractive error. In a new systematic review published in International Ophthalmology, researchers aimed to analyze the relationship between myopia and glaucoma, focusing on the structural and functional implications, risk factors and assessment modalities. They found the risk increased by approximately 20% per diopter of myopia, with a more pronounced increase in individuals with higher degrees of myopia.
The inclusion criteria consisted of studies published between 2012 to 2024 of subjects aged 18 years or older with high myopia, defined as a spherical equivalent of more than -6.00D or an axial length >26mm, diagnosed with chronic glaucoma. Various study designs were incorporated, including randomized controlled trials, prospective cohort studies and observational studies.
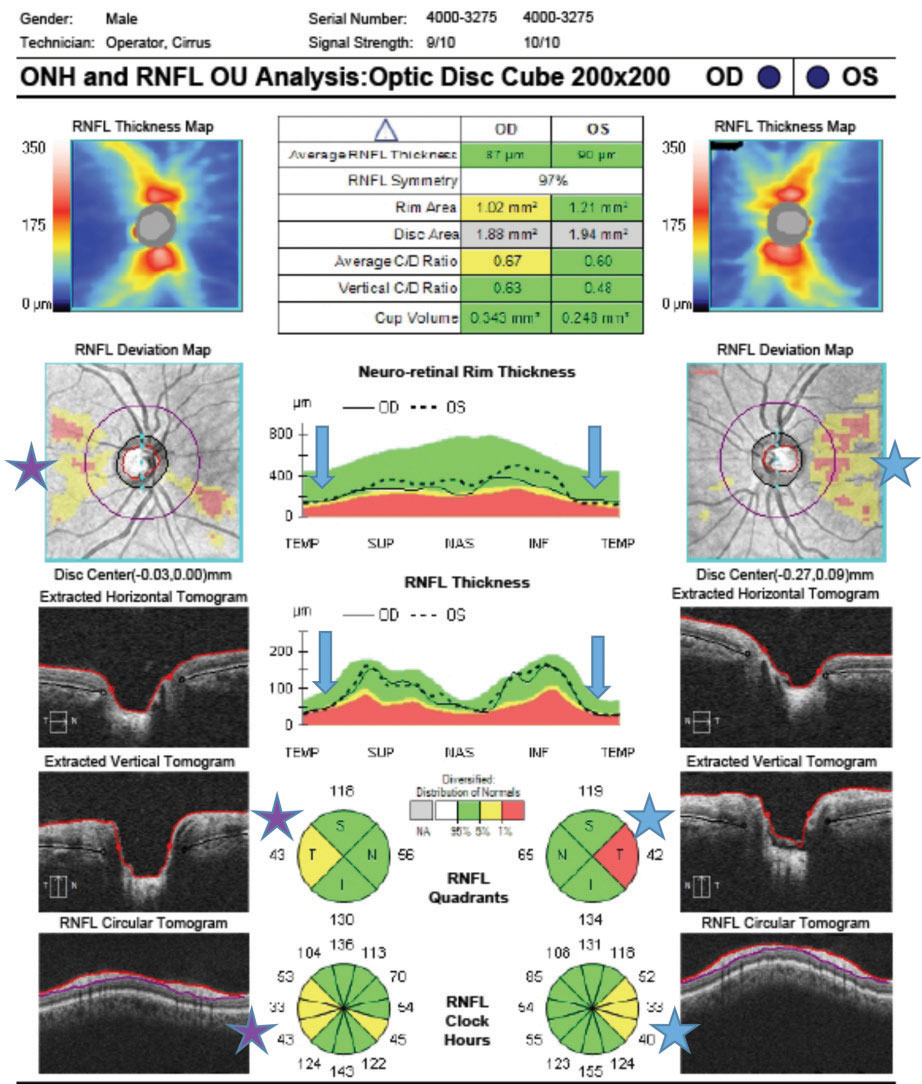
OCT played a crucial role in this study, particularly in highly myopic populations. OCT assessments revealed structural changes such as thinning of the retinal nerve fiber layer preceding functional losses. Structural changes associated with high myopia, such as elongation of the globe and thinning of the pRNFL, can exacerbate the vulnerability of the optic nerve to glaucomatous damage, the researchers explained in their paper on the work. “Longitudinal studies have shown that the progression of glaucomatous changes in myopic eyes can vary, with some studies reporting a greater rate of progression owing to the combined effects of myopia and glaucoma,” they wrote. “For example, longitudinal evaluations have indicated that myopic eyes with glaucoma exhibit a steeper decline in RNFL thickness than nonmyopic glaucomatous eyes, suggesting that myopia may be an additive risk factor for more rapid disease progression.” Also, glaucoma prevalence in myopic refractive surgery candidates is notably high, “underscoring the importance of vigilant screening in this population.”
Advanced imaging modalities, specifically OCT, is essential to optimize the detection and management of glaucoma in highly myopic individuals, because its ability to measure the pRNFL and GCC thickness allows for the early detection of structural changes that often precede functional loss, the authors explained. Enhanced-depth imaging OCT and OCT angiography have also been proven crucial for the detailed assessment of glaucomatous damage in myopic eyes.
“These imaging modalities are particularly valuable given the complex structural changes associated with high myopia, such as globe elongation and pRNFL thinning, exacerbating the risk of glaucomatous damage,” the authors explained in their paper.
“Although OCT remains the cornerstone of imaging in this context, integrating additional modalities, such as color fundus imaging, reflects the evolving landscape of diagnostic technologies,” the authors concluded. “Incorporating these advanced imaging tools is crucial for enhancing the specificity and sensitivity of glaucoma detection, thereby improving treatment outcomes in this high-risk population. Future research should refine these imaging techniques and develop specialized normative databases for highly myopic populations to address this subgroup’s unique challenges and enhance diagnostic accuracy and clinical management.”
| Click here for journal source. |
Quiroz-Reyes MA, Quiroz-Gonzalez EA, Quiroz-Gonzalez MA, Lima-Gomez V. Comprehensive assessment of glaucoma in patients with high myopia: a systematic review and meta-analysis with a discussion of structural and functional imaging modalities. Int Ophthalmol. October 11, 2024. [Epub ahead of print.] |


