Identifying patients with diabetes who are at high risk of developing diabetic retinopathy is crucial to intervention, and researchers are consistently looking at noninvasive imaging modalities to provide a closer look at the retinal microvasculature, specifically for quantification of retinal capillary hypoperfusion (ischemia) in the central retina. A new study published in Ophthalmology Science used swept-source and spectral-domain OCT-A, as well as widefield fundus fluorescein angiography (UWF-FFA), to reveal significant microvascular disease progression in eyes on the Diabetic Retinopathy Severity Scale (DRSS) of levels 47 (moderately severe) and 53 (severe), with the number of microaneurysms increasing with disease severity identified by color fundus photography.
 |
|
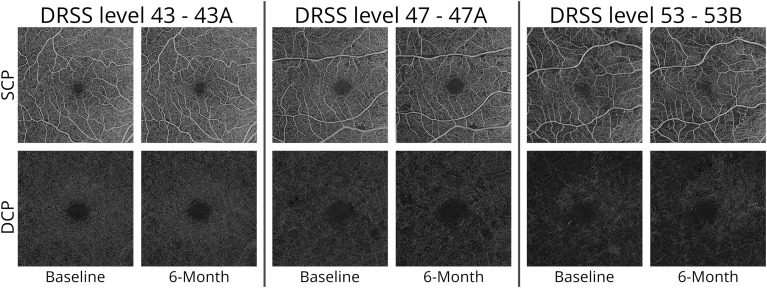
According to a recent study, OCT-A can play an important role in detecting microvascular changes in patients with moderate to severe NPDR. Researchers found that capillary hypoperfusion progresses significantly at advanced disease stages in the foveal avascular zone, skeletonized vessel density and perfusion density metrics for the inner and outer ring areas. They also discovered the rate of microaneurysms increases with disease severity. These findings could potentially pave the way for future clinical trials aimed at preventing the progression of diabetic retinopathy and its associated vision-threatening complications. This image from the study shows superficial and deep capillary plexus images acquired using swept-source OCT-A from patients with diabetic retinopathy severity levels 43, 47 and 53 in six-month intervals. Photo: Marques, Inês Pereira, et al. Ophthalmology Science. October 15, 2024. Click image to enlarge. |
This work is part of a two-year prospective longitudinal study, known as RICHARD, on the progression of perfusion in eyes with advanced stages of nonproliferative diabetic retinopathy (NPDR). These results, measured at participants’ six-month follow-up, show that OCT-A can discriminate eyes with advanced stages of NPDR, potentially opening up more ways to predict risk of progression, according to the paper’s authors.
The six-month results included 51 eyes. Twelve eyes (23.5%) were classified as DRSS level 43 (moderate NPDR), 30 eyes (58.8%) classified as DRSS level 47 and 9 eyes (17.7%) as DRSS level 53. Swept-source OCT-A metric showed statistically significant differences in the foveal avascular zone metrics and in both skeletonized vessel density (SVD) and perfusion density (PD) metrics for the inner and outer ring areas. Spectral-domain OCT-A showed statistically significant differences only in the SVD and PD metrics for the inner and outer ring areas. The authors also mention it’s noteworthy that progression of capillary hypoperfusion was identified by the swept-source device in eyes with DRSS levels 47 and 53, but not in DRSS level 43.
There were no statistically significant differences in BCVA over the six-month period in the three DRSS levels, according to the study. Changes in structural metrics over six months weren’t detected either, including central retinal thickness and ganglion cell layer/inner plexiform layer thickness.
“Our results show that the capillary hypoperfusion in the DRSS levels 43 and 47 progresses by involving preferentially the DCP in the outer ring of the central retina until it appears to stabilize in the DRSS level 53,” wrote the authors in their paper on the study. “In contrast, the number of microaneurysms increases progressively through DRSS levels 43, 47 and 53” apparently in association with the presence of intraretinal microvascular abnormalities in DRSS levels 47 and 53.
“Our study also showed that the ischemic index obtained using UWF-FFA demonstrates the presence of capillary closure and hypoperfusion but is much less discriminative than the OCT-A metrics obtained using the noninvasive SS-OCT-A,” they continued. “Furthermore, demarcating nonperfusion in FFA images is subjective, while OCT-A metrics are automatically extracted.”
The authors hope this study sheds light on detecting and understanding disease progression, saying, “In the current analysis we found that progression of the preproliferative stage of diabetic retinopathy can be detected based on retinal microvascular metrics obtained with OCTA, a non-invasive imaging procedure, in a six-month interval. These results open the door for future interventional trials targeting retinal capillary closure and ischemia as well as addressing the subsequent hyperperfusion response.”
The authors concluded, “The ability to monitor the balance between the initial hypoperfusion stage and the hyperperfusion response using metrics of capillary perfusion obtained with noninvasive OCT-A imaging and microaneurysm counting open ways to predict risk of progression to proliferative diabetic retinopathy in a given eye, with moderate-severe nonproliferative retinopathy.”
| Click here for journal source. |
Marques, Inês Pereira, et al. Progression of capillary hypoperfusion in advanced stages of nonproliferative diabetic retinopathy: Six-month analysis of RICHARD study. Ophthalmology Science. October 15, 2024. [Epub ahead of print]. |


