 |
|
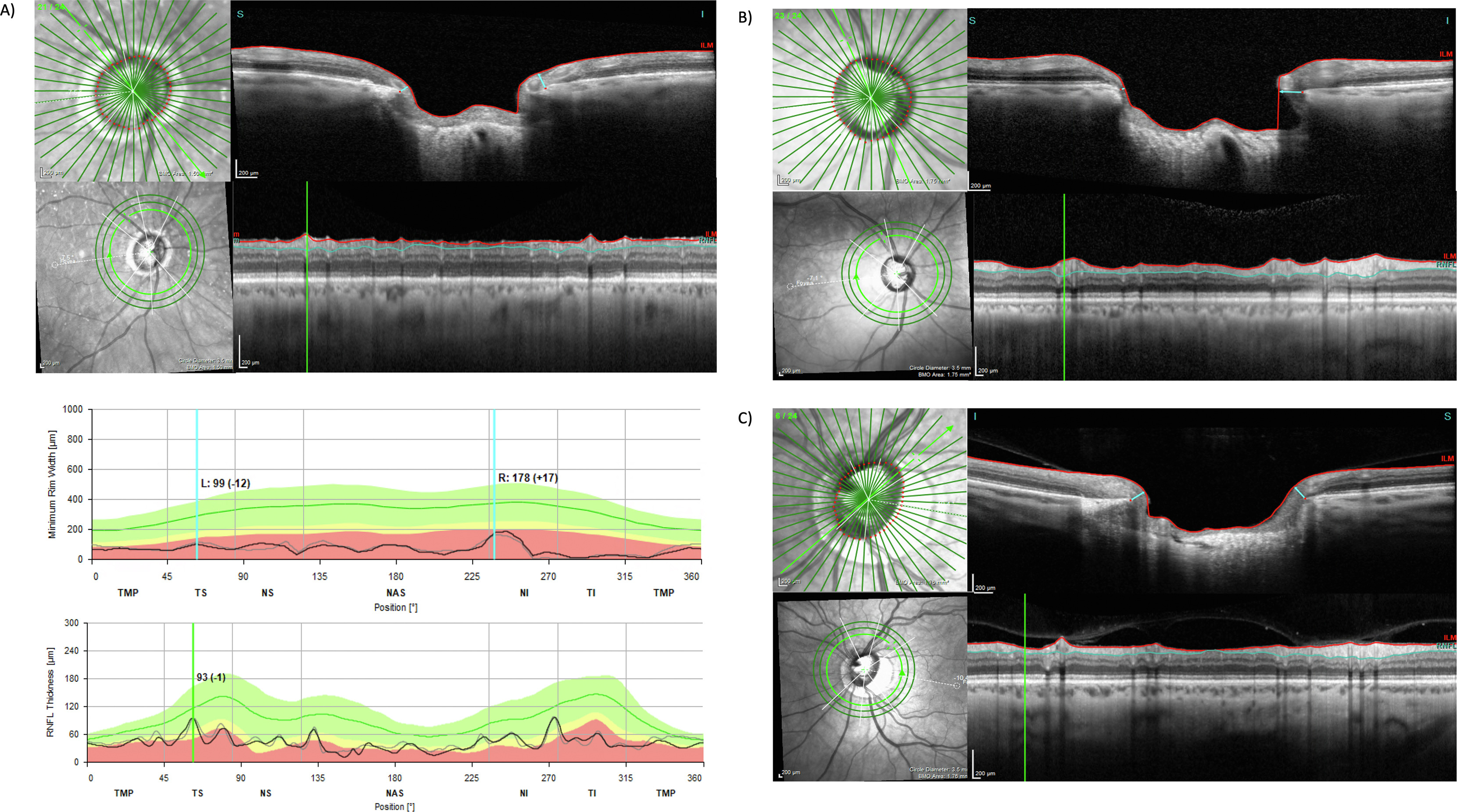
Among a cohort of glaucoma patients from the Advanced Glaucoma Progression Study, researchers found an overall low rate of mismatches involving BMO-MRW and RNFL thickness (8%), 80% of which were attributed to retinal blood vessels. These images from the paper show (A) how a large blood vessel thickens the RNFL more than the BMO-MRW at the 60° sector, (B) how a large blood vessel preferentially thickens the RNFL at the 75° sector due to the angular offset between the site of vessel insertion at the optic nerve head and the trajectory of the vessel in the retina and (C) how a small blood vessel preferentially thickens the BMO-MRW at the 52.5° sector. Photo: Zhuang I, et al. Ophthalmol Sci. August 21, 2024. Click image to enlarge. |
Among the key OCT biomarkers for tracking glaucoma progression is circumpapillary retinal nerve fiber layer (RNFL) thickness. More recently, the Bruch’s membrane opening minimum rim width (BMO-MRW)—which measures the shortest distance from the inner opening of the Bruch’s to the internal limiting membrane—has emerged as a significant biomarker for detecting and monitoring glaucoma due to its ability to provide a more precise evaluation of the neuroretinal rim or the retinal ganglion cells axonal structure in an eye. Studies comparing these two biomarkers in terms of diagnostic accuracy and their correlation with structural changes have shown varied results. Thus, researchers from Jules Stein Eye Institute at UCLA sought to investigate the discrepancies between RNFL and BMO-MRW measurements among glaucoma patients as well as possible anatomical factors contributing to these differences.
The cross-sectional observational study included 186 eyes (118 patients) with glaucoma enrolled in the Advanced Glaucoma Progression Study. OCT optic nerve head volume scans from the final available visit of each patient were used for analysis. Only patients with RNFL or BMO-MRW measurements below the first percentile on the temporal-superior-nasal-inferior-temporal curve were included.
Mismatch analysis showed that discrepancies between RNFL and BMO-MRW measurements occurred in 8% of sectors. Mismatches where BMO-MRW was high but corresponding RNFL was low were primarily found in the 45° and 322.5° sectors. Conversely, mismatches where RNFL was high but corresponding BMO-MRW was low were most prevalent at the 75° sector.
The researchers found that retinal blood vessels accounted for 80% of the observed mismatches. Among mismatches of high RNFL with low BMO-MRW, 91% were due to large blood vessels. For mismatches involving high BMO-MRW with low RNFL, 63% were associated with small to large blood vessels. The remaining discrepancies were linked to retinoschisis or the inclusion of outer retinal layers in the BMO-MRW measurements.
The finding that the major branches of the central retinal artery and vein were responsible for nearly all high RNFL vs. low BMO-MRW mismatches “also [explains] why these mismatches were predominantly located along the superior and inferior poles of the optic nerve head,” the researchers commented in their paper, published in Ophthalmology Science. “These larger vessels typically lead to a more extensive thickening of the RNFL relative to the BMO-MRW as they are largest near the optic nerve head poles and the RNFL bundles tend to follow their course,” they wrote, adding that “in fact, Hood et al. have shown that roughly 13% of the total circumpapillary RNFL thickness is accounted for by blood vessels.”
Conversely, the high BMO-MRW with low RNFL group “had a smaller contribution from blood vessels (63%), with a more significant influence originating from small circumlinear vessels,” the researchers explained. “These vessels led to an increase in the BMO-MRW thickness without a corresponding thickening of the RNFL.”
Since small vessels within the optic nerve head appear to lead to BMO-MRW thickening, and large vessels appear to thicken the RNFL, the study authors suggest that using these parameters in conjunction could allow one to compensate for the deficiencies of the other.
“The combined structural information from these techniques provides a more comprehensive assessment of glaucomatous damage, enabling earlier diagnosis and more precise monitoring of disease progression, especially in advanced stages,” they concluded in their paper. “Further advancements in the OCT technology could be useful in eliminating the effect of large blood vessels on the RNFL measurements and small blood vessels on the BMO-MRW measurements.”
Zhuang I, Ashrafkhorasani M, Mohammadzadeh V, Nouri-Mahdavi K. Sources of discrepancy between retinal nerve fiber layer and bruch’s membrane opening-minimum rim width thickness in eyes with glaucoma. Ophthalmol Sci. August 21, 2024. [Epub ahead of print]. |


