 |
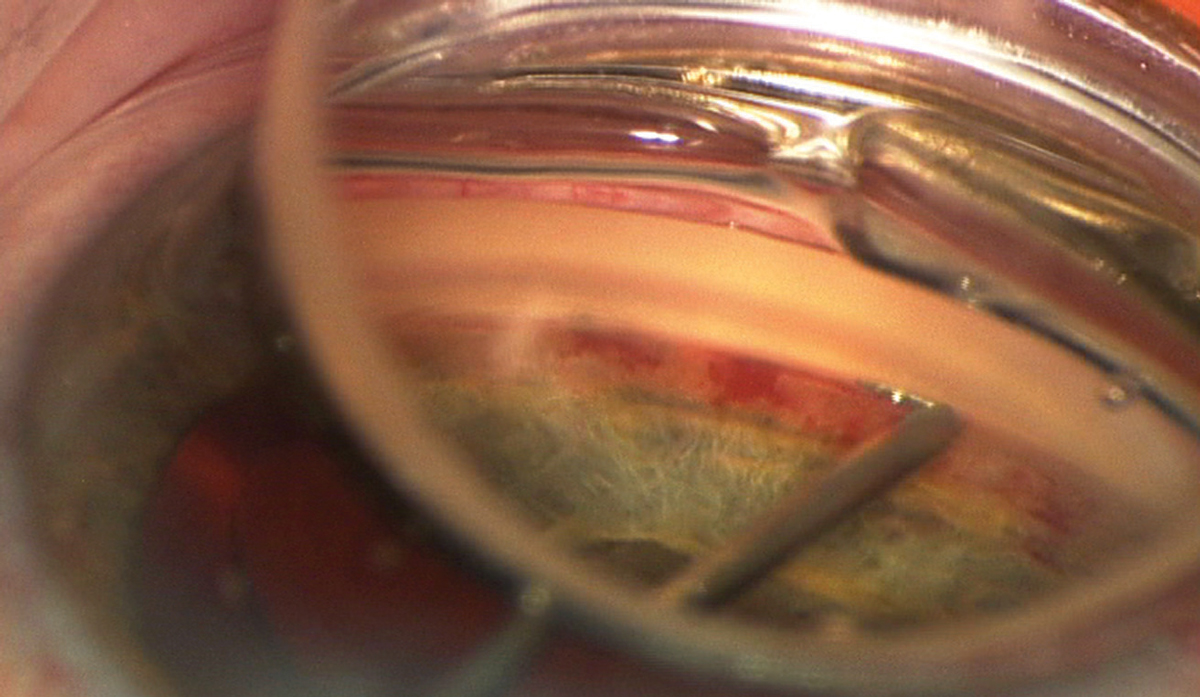
| The incidence of MIGS procedures for the Black cohort in this study was lower compared to those of other races, except when treating patients with a transluminal dilation of Schlemm’s canal without device or stent retention. Black patients were more likely to receive this for the treatment of mild to moderate primary open-angle glaucoma. Photo: Joseph W. Sowka, OD. Click image to enlarge. |
Inequalities in access to healthcare can lead to higher risk for disease and inadequate care for certain populations. For instance, Black patients in particular are at a higher risk for glaucoma and yet tend to not receive proper care for their condition. Minimally invasive glaucoma surgery (MIGS) has seen huge uptake by surgeons in the last decades but how often are ophthalmologist offering this treatment for Black individuals?
A study recently published in the American Journal of Ophthalmology reported on the racial disparities found in the incidence of MIGS for managing patients with primary open-angle glaucoma. Using a database of over 100 million electronic medical records from 64 healthcare organizations, researchers assessed the incidence of MIGS within one year for 63,418 primary open-angle glaucoma cases.
“We found that African American patients with mild-moderate primary open-angle glaucoma were significantly less likely to undergo microinvasive glaucoma surgery procedures as opposed to their non-African American counterparts,” wrote the researchers in their paper for this study. “This finding highlights an important area for providers to remain cognizant of as treatment regimens are formulated for future vulnerable patients.”
To find these results, the researchers divided the subjects equally into two cohorts: Black subjects and non-Black ones. Overall, 1,268 cases in the Black cohort received a MIGS procedure within one year, while 1,508 cases in the non-Black cohort met the same outcome.
The researchers were limited in their research due to a few factors. Each electronic medical record from the database was filled out using ICD-10 classification and CPT codes, so the researchers had to presume that physicians properly followed billing practices and uniform diagnosis patterns during examination. And since the data was collected from elsewhere, specific clinical features were not assessed in this study, such as intraocular pressure, cup-to-disc ratio, corneal thickness and visual field index. Additionally, this data did not list glaucoma patients who are uninsured or unable to see a provider, thus skewing the results. The odds ratio for a Black glaucoma patient to receive MIGS relative to others was 0.834.
“Future studies may be helpful to assess specific clinical features such as intraocular pressure, cup-to-disc ratio, and visual field index of patients with primary open-angle glaucoma diagnosis to gather an enhanced understanding of treatment regimens,” concluded the researchers in their paper for this study. “Additionally, it would be beneficial to expand social demographics beyond race to encompass living situation, socioeconomic status, and education to further investigate relationships between primary open-angle glaucoma diagnosis and treatment regimens.”
| Click here for journal source. |
Vasu P, Hall RP, Wagner IV, et al. Racial disparities in microinvasive glaucoma surgery for management of primary open-angle glaucoma: A propensity matched cohort study. American Journal of Ophthalmology. October 3, 2024. [Epub ahead of print]. |


