 |
|
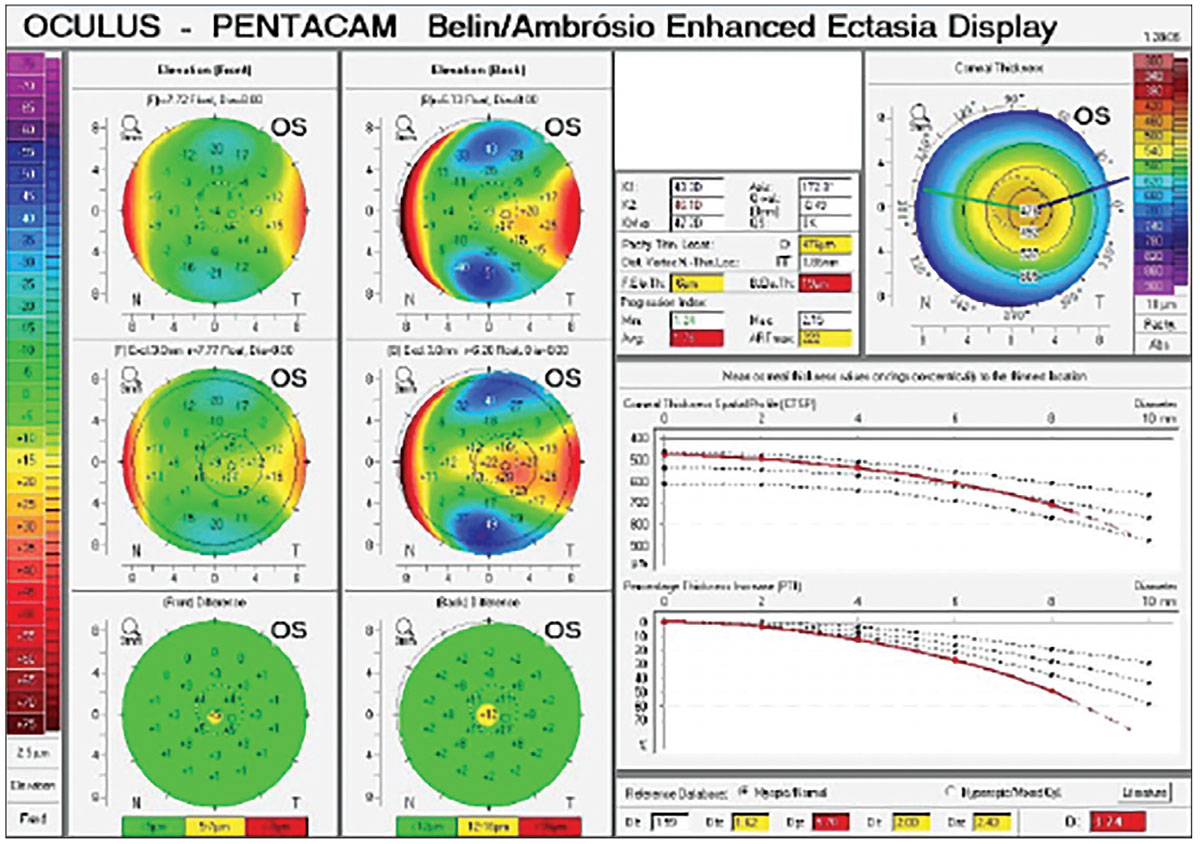
A recent investigation found useful alterations in the corneal indices, keratometries of progression and the ABCD grading system in six-month post-CXL patients with keratoconus. Photo: Julie Song, OD. Click image to enlarge. |
Kmax is the most common metric for ectatic progression detection and monitoring, as well as for assessing the effectiveness of crosslinking (CXL) against keratoconus. However, studies have revealed that the Kmax does not accurately indicate the severity of ectasia, and ectatic progression can occur even without a change in the Kmax. Although many more recent techniques use complicated keratometric indices to characterize progression, earlier systems relied solely on serial topographic analyses to describe progression. The Belin ABCD keratoconus staging approach was created to use the thinnest areas of the cornea to identify any manifestation within the anterior and posterior curves of the cornea. In a recent study published in Clinical Ophthalmology, researchers in Saudi Arabia assessed changes in corneal parameters six months after corneal crosslinking for progressive keratoconus using the ABCD system. They found that, throughout the six-month postoperative follow-up, parameters A, B and C exhibited statistically significant changes. Parameter A increased six months after surgery, whereas parameters B and C decreased. However, parameter D did not have a statistically significant change.
The ABCD grading system divides keratoconus into five stages, based on structural and functional alterations, by using tomographic measures and visual acuity. It gathers information on A (anterior radius of curvature), B (posterior curvature), C (corneal thickness) and D (corrected distance and visual acuity) in the 3.0mm zone centered on the thinnest part of the cornea. This study included 16 eyes of 16 patients with keratoconus who underwent corneal CXL at the same hospital and were at least 18 years old. At least one preoperative and one postoperative examination was performed for each patient. Six months after the procedure, patients underwent corneal tomography.
Other parameters monitored included maximal keratometry (Kmax) (K1 and K2), Belin/Ambrósio Enhanced Ectasia Display and index vertical asymmetry. Preoperatively and six months after surgery, Kmax, K1 and Belin/Ambrosio-enhanced ectasia demonstrated substantial differences. K2 and the average pachymetric progression index did not change significantly.
“Conducting a study in Saudi Arabia to assess the effectiveness of CXL in progressive keratoconus by using the ABCD grading system can fill a gap and provide regionally specific data,” the study authors wrote in their paper. “By offering regional perspectives on how local patients would respond, it could contribute to the development of locally adapted treatment protocols and improve clinical outcomes in patients with keratoconus.”
The team recognized their study’s small sample size and short follow-up time. Still, they noted that anterior and posterior corneal curvatures and corneal thickness profiles can be useful for monitoring the progression of keratoconus and the success of corneal CXL.
Alzahrani M, Alammari O, Binyamin A, et al. Assessment of corneal crosslinking effect on progressive keratoconus by using the ABCD grading system. Clin Ophthalmol. 2024;18:2349-55. |


