 |
|
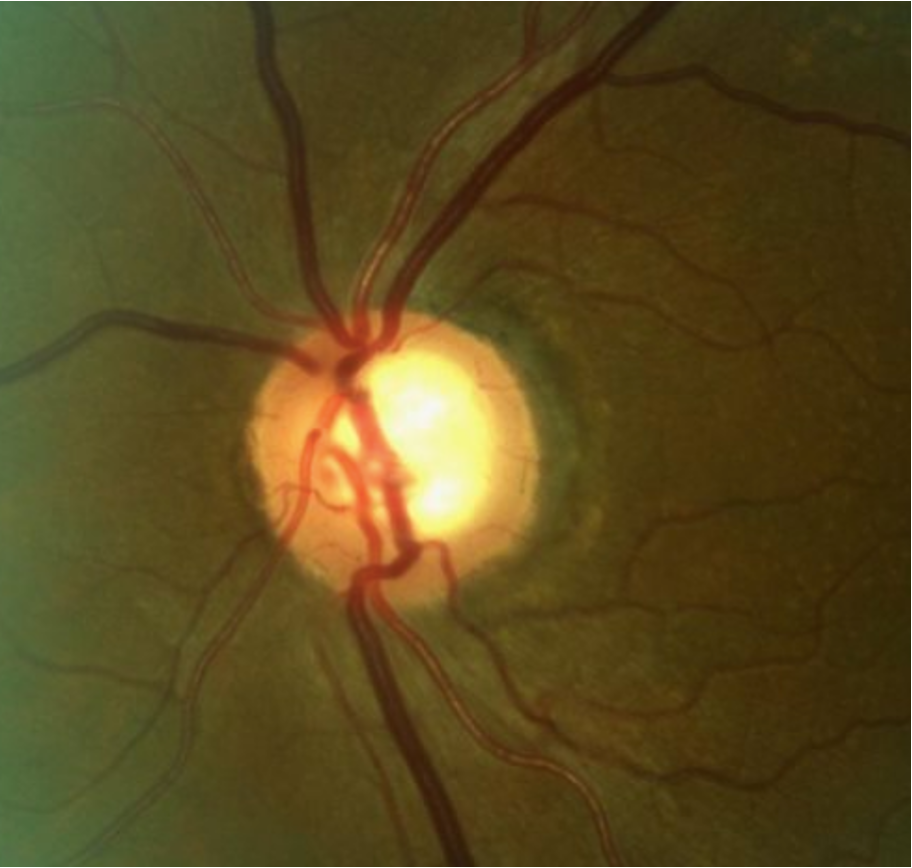
Patients with anterior chamber VEGF-A levels above 148.5pg/ml were found to have an almost 10-fold greater likelihood of glaucoma than controls. Photo: Andrew Rixon, OD. Click image to enlarge. |
The purpose of a new cross-sectional study conducted in Greece was to compare VEGF-A levels in the aqueous humor of patients with primary open angle glaucoma (POAG) and non-glaucomatous eyes. The authors found that VEGF-A is elevated in POAG patients, with various retinal cells possibly contributing to VEGF-A production.
Aqueous humor samples (50μl to 100μl) were obtained from 76 participants—39 with POAG and 36 with age-related cataracts as controls—from the anterior chamber at the start of glaucoma or cataract surgery. The POAG group received topical anti-glaucoma medications, had regulated IOP and had no other ocular disease. The control group consisted of patients with no other ocular pathology except age-related cataracts.
VEGF-A levels were significantly elevated in the POAG group (166.37 ±110.04pg/ml) compared to the control group (119.02 ±49.09pg/ml). An optimal cut-off for use as a biomarker of disease was found to be 148.5pg/ml, with a positive prognostic value of 75% and negative prognostic value of 62.5%. After adjusting for sex and age, patients with VEGF-A higher than 148.5pg/ml had almost 10 times greater likelihood for POAG.
These findings align with the authors’ previously published meta-analysis that suggested a tendency toward heightened VEGF-A levels in POAG. They are also consistent with other studies reporting statistically significant increase in VEGF-A levels among patients with POAG.
“However, it’s worth noting that certain studies did not depict any statistical difference in VEGF-A levels among POAG, while two studies have described decreased VEGF-A levels in patients with POAG with statistically significant difference,” the authors noted in their paper for the journal In Vivo. “It’s important to highlight that the aforementioned studies examined smaller cohorts of patients, ranging from 31 to 56 individuals in total, whereas our study enrolled a larger cohort of 76 participants.”
The authors offered two potential reasons why VEGF-A levels might be elevated in eyes with glaucoma, the first being that various retinal cells may contribute to VEGF-A production. “Froger et al. have shown in vitro that retinal ganglion cells can produce VEGF-A, serving as an autocrine factor to promote their own survival via the VEGFR-1 pathway,” the authors explained. “Additionally, the microglial cells were found to produce substantial levels of VEGF-A acting as a paracrine neuroprotective factor for retinal ganglion cells in vitro. Supporting the above hypothesis, a recent meta-analysis revealed a significant reduction in the RNFL-thickness six and 12 months after the injection of ant-VEGF agents, as well as at the end of the follow-up period.”
Secondly, the trabecular meshwork (TM) cells could be considered as another source of VEGF-A, according to the authors. “Reina-Torres et al. have demonstrated in vitro that TM cells secrete VEGF-A in response to mechanical stretch, mimicking elevated IOP and acts as a paracrine regulator of conventional outflow activity,” the authors explained in their paper. “This action of VEGF-A is mediated via the VEGFR-2 pathway at the level of Schlemm’s canal endothelium.” The team cites a study by Fujimoto et al. showing in vitro that VEGF-A regulates conventional aqueous outflow of Schlemm’s canal endothelial cells through VEGFR-2 signaling.
Based on the in vitro studies mentioned above, the authors hypothesize that the overexpression of VEGF-A targets the survival of retinal ganglion cells and/or the viability of conventional aqueous outflow.
“VEGF-A is emerging as a key mediator molecule that is implicated in many biological procedures,” the authors concluded. “We strongly believe that research interest should focus beyond its well-known and well-described angiogenic activity. More in vivo studies are needed in order to establish its potential key role in POAG as a neuroprotective factor.”
Dimtsas G, Ieronymaki A, Chatzistefanou KI, et al. Elevated VEGF-A levels in the aqueous humor of patients with primary open angle glaucoma. In Vivo. 2024;38(4):1875-81. |


