As dry eye disease is frequently underdiagnosed in pediatric patients, researchers from Illinois College of Optometry aimed to characterize meibomian gland morphological abnormalities (specifically, atrophy and tortuosity) and identify risk factors for the same in children. They found that elevated body mass index, an unhealthy diet and reduced outdoor activity are risk factors in children, according to a paper published last week in Optometry & Vision Science. A preliminary report on the research was also presented at this year’s ARVO conference.
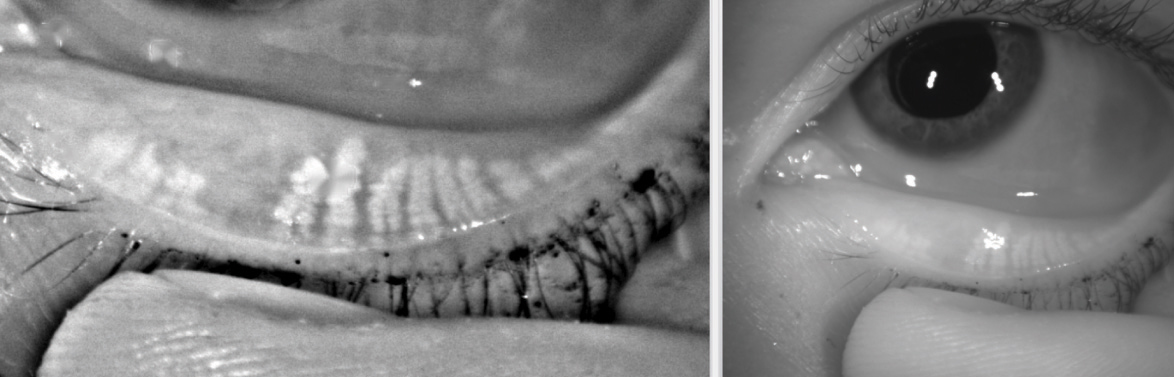 |
| Findings from this study suggest that eyecare practitioners should assess meibomian gland dysfunction and screen for morphological changes such as gland atrophy even in children. Photo: Kambiz Silani, OD. Click image to enlarge. |
A total of 160 children (84 female, 76 male), primarily African American and Hispanic, between the ages of five and 18 underwent a comprehensive eye exam including slit lamp examination to evaluate the meibomian glands, conjunctival papillae and tear film. Infrared photography was performed, including assessment of noninvasive tear film breakup time and tear meniscus height. Meibomian gland atrophy and tortuosity were assessed. A modified Ocular Surface Disease Index (OSDI) survey was administered along with surveys on screen time, diet and outdoor activity.
One of the authors of this study, Lindsay Sicks, OD, explains that severe meibomian gland atrophy was noted in at least one eyelid in 31% of participants and severe gland tortuosity was found in at least one eyelid in 84% of subjects.1 “Not all eyecare practitioners will have access to infrared meibomian gland imaging; however, our study suggests that a more thorough evaluation of dry eye and meibomian glands in children could be beneficial,” Dr. Sicks says.
Risk factors included BMI associated with gland atrophy, poor diet (survey of consumption of sugary drinks and fast food per week) associated with gland tortuosity and outdoor activity level associated with gland atrophy.
The mechanism for the findings is unclear and further analysis is needed to uncover the etiology of the meibomian gland morphological changes in children and their connection to BMI and dry eye, Dr. Sicks emphasizes. “It is possible that in patients with higher BMI, an altered systemic lipid profile can affect the meibum lipid concentration, thus affecting the viscosity of the meibum and therefore the gland obstruction and morphology,” she explains, pointing to a 2010 study by Dao et al. to that effect.2
Dr. Sicks adds that at this time, these findings are not applicable to adults with high BMI. “I don't think we can extrapolate what we find in our particular pediatric population to the general adult population at this point,” she observes. “The OSDI survey used in this study was modified to be relevant to children, so this could have affected the overall results. We do not have validated cutoffs for many diagnostic tests in children nor symptom questionnaires that have been validated in a pediatric population. This is an area for further future study.”
|


