 |
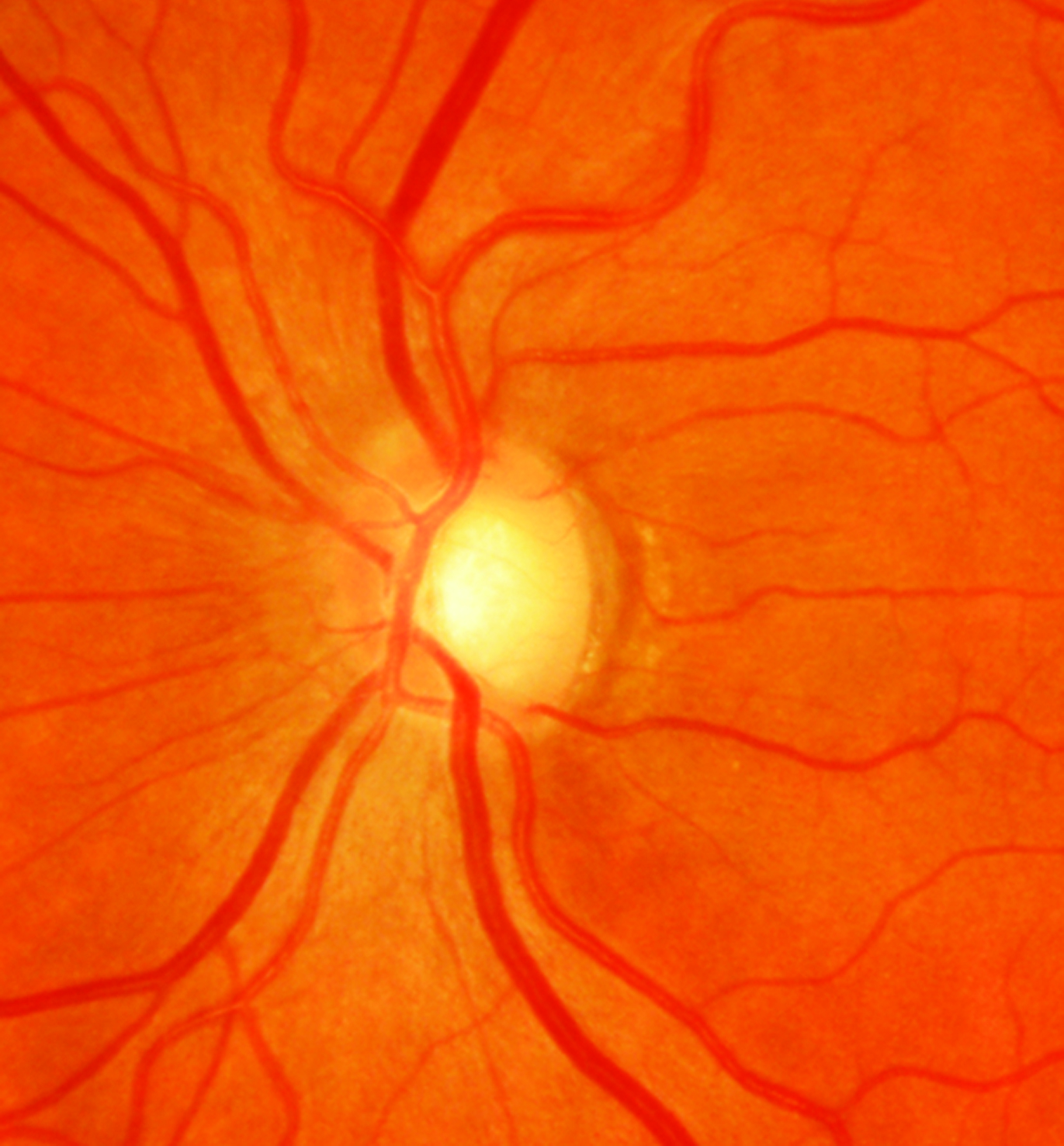
| Poor sleep duration confers a 1.66-fold higher risk of POAG, according to this study. Photo: Sarah B. Klein, OD. Click image to enlarge. |
The early bird gets the… glaucoma? Maybe so, says a new study.
Previous research has investigated the connection of glaucoma with sleep behavior, but any causal relationship has remained largely unclear. A novel study aimed to elucidate just that by analyzing genetically predicted sleep traits with primary open-angle glaucoma (POAG) using a two-sample bidirectional Mendelian randomization method. In other words, it tested the association of POAG and sleep trouble for cause-effect dynamics in either direction.
The bidirectional analysis included data from publicly available genome-wide association studies of European descent. The researchers’ results indicated a positive correlation between genetically predicted ease of getting up in the morning and sleep duration with POAG. The adverse effects of these two traits on POAG persisted after adjusting for factors of BMI, smoking, drinking and education, thus strengthening the evidence that genetic liability to poor sleep traits is in fact a risk factor of POAG. However, the relationships between genetic liability of POAG and different sleep behaviors were not significant in the opposite direction.
POAG may not change sleep-related behaviors, but the study authors noted in their paper for Nature and Science of Sleep that “although there was no potential causal inference between these genetically predicted sleep traits and POAG, we still need to pay attention to sleep-related health to mitigate the incidence of POAG.”
Upon further discussion, the authors point to multiple studies indicating similar relationships or connections. Poor sleep quality and disruption are commonly observed in POAG and glaucoma patients; one study indicated glaucoma patients scored worse compared with controls for sleep latency, sleep duration and subjective sleep quality.
The authors offer an explanation for this observed relationship, caused by underlying mechanisms between sleep-related behaviors and POAG that biologically makes sense. One possibility is the pathogenetic mechanism involving systemic inflammation-related processes, such as C-reactive protein, neutrophil-to-lymphocyte ratio, systemic immune inflammation index and cytokine TNF-α, which are relevant to vision in POAG. Recurrent hypoxia with increased vascular resistance and oxidative stress damage to the optic nerve are both vascular factors that have shown implication in POAG pathogenesis.
Yet another possibility has to do with chronic insomnia. Its related physiological responses may stimulate neurotransmitter secretion as well as activating the autonomic nervous system, thus affecting intraocular pressure (IOP) regulation and optic nerve perfusion. Comorbidities may further lead to this observation, as mood disorders like anxiety and depression often occur with insomnia and may result in IOP elevation through dysregulated levels of the hormone cortisol.
The authors conclude that their analysis indeed demonstrates ease of getting up in the morning and poor sleep duration are indicative risks of POAG. “To better understand and manage both phenotypes in our clinical implications, potential ophthalmologic screening and intervention among individuals with chronic sleep problems should be made to help prevent POAG,” they advise. Doctors can consider incorporating questions about sleep patterns and behaviors into routine patient assessments, especially for individuals at higher risk for POAG. This can help identify patients who may be at increased risk and may benefit from further evaluation. For patients already diagnosed with POAG, consider discussing sleep patterns and behaviors as part of the overall management plan.
Zhang J, Chen X, Zhu Y, et al. Investigating the causal relationship between sleep behaviors and primary open-angle glaucoma: a bidirectional two-sample Mendelian randomization study. Nat Sci Sleep. 2024;16:143-53. |


