 |
|
High blood pressure increased ciliary artery pressure in the eye, elevating ultrafiltration and the production of aqueous humor, which has been thought as the cause for increased IOP, thus hypertension being important to check for. Photo: Mayo Clinic. Click image to enlarge. |
Glaucoma has many factors that contribute to its development, of course. However, one of the most important aspects to look for is intraocular pressure (IOP). As high IOP is closely related to glaucoma., understanding what contributes to elevation may help clinicians monitor and educate patients.
In a new study appearing in the Journal of Glaucoma, researchers analyzed the association of the STOP-BANG questionnaire score—widely used as a screening tool to determine a person’s risk of having obstructive sleep apnea (OSA)—with IOP measurements. Korean adults aged 40 or older were included, totaling 6,315 individuals. OSA risk was measured with the STOP-BANG questionnaire and IOPs were measured with a rebound tonometer. IOP quartile association was analyzed with OSA risk after adjusting for factors of sociodemographic characteristics, lifestyle and diabetes.
The researchers observed that for participants with a STOP-BANG score of three or greater, the ratio for high IOP was 1.27, or 27% higher, when compared with those with a score of zero to two. What’s more, the odds ratio for high IOP increased just as score did, with a 1.95 odds ratio of high IOP in the group of those with STOP-BANG scores of six to eight when compared with those of a zero score.
Individuals who had loud snoring, observed breathing interruptions during sleep, hypertension or a wide neck circumference (≥40cm) experienced 24% to 40% higher odds of having elevated IOP than those without these characteristics. For those who possessed all four of these factors, the odds ratio of high IOP was 2.09 times higher, or more than double that of the group without these factors.
Due to these results, the study authors write that they “support our hypothesis that high IOP is associated with high STOP-BANG scores but that this association varies depending on the components of STOP-BANG; that is, the association with high IOP varies depending on which components make up the STOP-BANG score.”
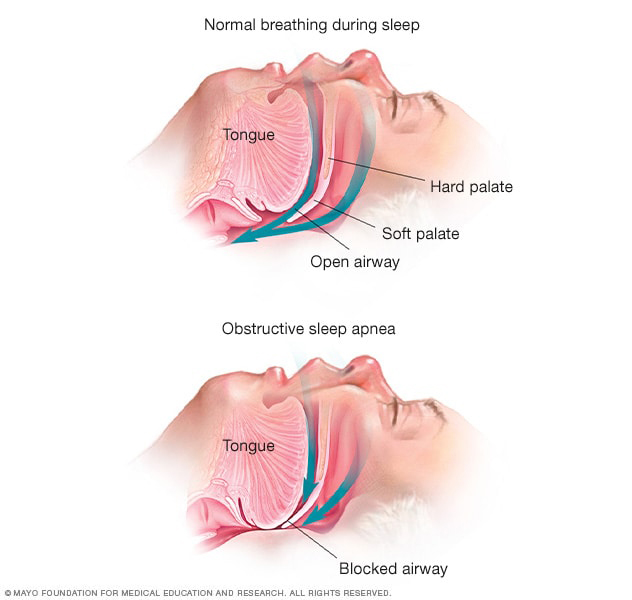
The authors expound that instead of using BMI as a risk parameter for IOP measurements, they instead used neck circumference, which is an index of upper body obesity and which positively correlates with changes in systolic and diastolic blood pressure as well as other components of metabolic syndrome. Association with high IOP may stem from obesity-related fat deposition in the neck. This can cause narrowing of the pharyngeal lumen, thus resulting in obstruction when sleeping and venous engorgement, then causing an increase in episcleral venous pressure and leading to reduced aqueous outflow related to high IOP.
The authors continue in their discussion to reflect on how, “from a public health perspective, these findings suggest the need for IOP measurement in individuals with high STOP-BANG scores” and comment that “while snoring and other sleep-disordered breathing symptoms (as assessed by the STOP-BANG questionnaire) may not yet be routinely assessed in ophthalmic practice, there is a growing body of evidence supporting the potential impact of OSA on eye health, including ocular health.”
| Click here for journal source. |
Kim JL, Lee K. Association between risk of obstructive sleep apnea and intraocular pressure based on the Korea National Health and Nutrition Examination Survey VIII. J Glaucoma. October 30, 2024. [Epub ahead of print]. |


