 |
|
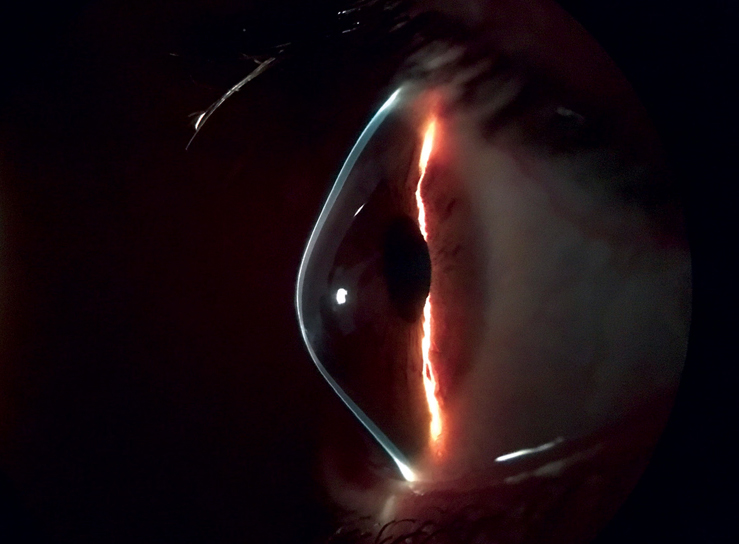
Atopic dermatitis, or eczema, is not only a contributor to the risk of keratoconus, but also a causal effect on the disease. Photo: Brian Chou, OD, and Jerome Legerton, OD. Click image to enlarge. |
The literature on atopic dermatitis explains how this condition is sometimes associated with risk of keratoconus, and that higher incidence rates of keratoconus have been reported in patients with eczema. However, not enough has been reported on potential causal relationships between the two diseases. To further investigate this association, researchers from China recently conducted a Mendelian randomization study.
What is a Mendelian randomization study? According to the researchers, this unique statistical method uses single nucleotide polymorphisms, the most common type of genetic variation in people, to estimate whether there’s a causal relationship between the exposure (atopic dermatitis) and the outcome (keratoconus). This allows investigators to limit the influence of confounders and/or reverse causation that may happen regularly in more common observational studies.
After identifying a total of 22,474 cases for their dataset, the researchers began their analysis. Basically, the researchers plugged their data into a statistical analysis package designed for such purposes. This program made all causal inferences for the relationship between the exposure and outcome, and further strengthened the study by using a host of Mendelian randomization study methods in a two-sample approach. The analysis revealed significant evidence that atopic dermatitis has a causal effect on keratoconus and displayed consistent results to that effect throughout the study. Only after performing a reverse Mendelian randomization analysis did the researchers discover that keratoconus does not have a causal effect on eczema.
“We recommend that individuals with atopic dermatitis undergo regular ophthalmic examinations, such as corneal thickness and cornea topography, to detect any early signs of keratoconus,” suggested the researchers in their study, published recently in Translational Vision Science & Technology. “Especially for young patients, receiving ophthalmic examinations and treatment upon the diagnosis of atopic dermatitis can help to prevent permanent ocular damage threatening vision.”
In their paper, the researchers cite evidence in previous studies suggesting that some combination of eye rubbing, systemic inflammation and genetic factors present in those with atopy conspire to induce corneal shape changes characteristic of keratoconus.
There were some limitations that may have skewed the results in this study. The researchers cited that their dataset did not have a diverse population, and that all participants were of European decent. Further genetic data will need to be analyzed in future studies. Additionally, this investigation ruled out possible pleiotropic effects even though they are important to recognize in a clinical setting. They were removed by the Mendelian randomization program during analysis.
“In conclusion, using a two-sample Mendelian randomization approach, our study strongly supported previous observational studies suggesting that atopic dermatitis has unidirectional causal effects on keratoconus,” concluded the researchers in their paper on the study.
Chang Y, Huang T, Yang S, et al. Causal association between atopic dermatitis and keratoconus: A Mendelian randomization study. Translation Vision Science and Technology 2024;13:9:13. |


