 |
|
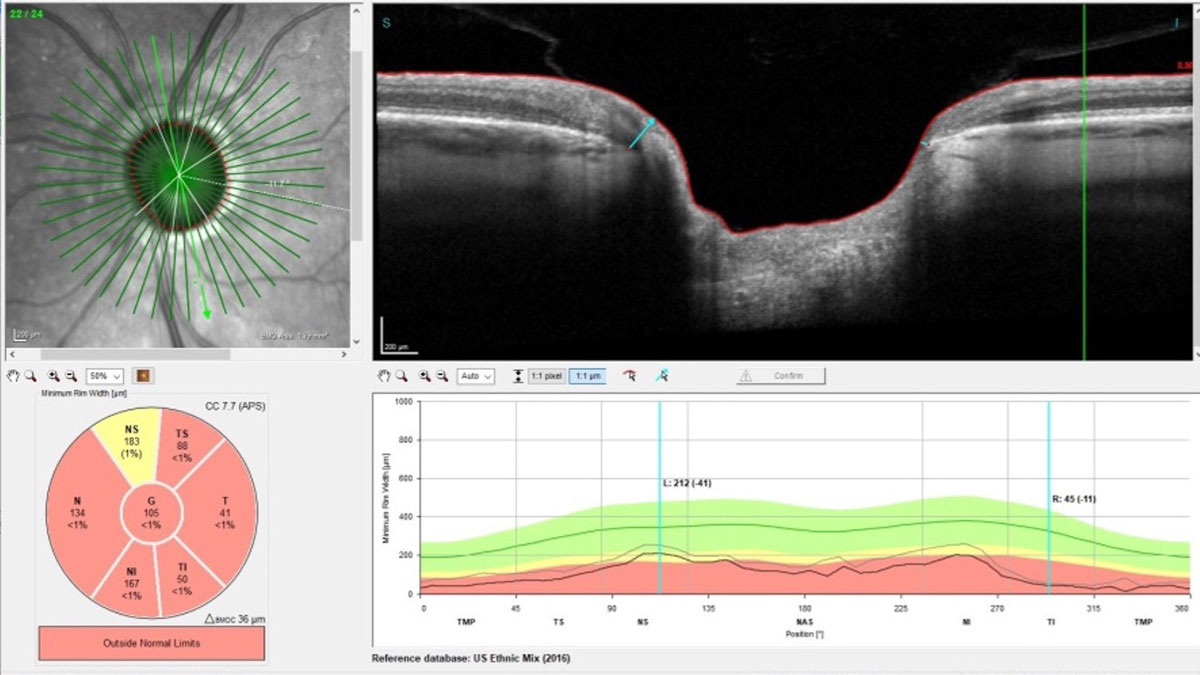
The study determined high polygenic risk for primary open-angle glaucoma was associated with increased risk for and earlier development of POAG in patients with ocular hypertension, suggesting the potential for more personalized disease treatment in this population. Photo: James Fanelli, OD. Click image to enlarge. |
Despite primary open-angle glaucoma (POAG) accounting for 69% of the disease’s prevalence globally, intraocular pressure (IOP) is still the only risk factor that can be modified with the help of therapeutics or surgery. However, as genetic research advances, the medical community is increasing its identification of variants that contribute to the development of POAG and attempting to aggregate them into a polygenic risk score (PRS) suitable for clinical application. PRS has been associated with diseases such as coronary artery disease, type II diabetes, macular degeneration and diabetic retinopathy, among others. A new study explored the relationship between ocular hypertension (OHT), high PRS and progression to POAG.
The post hoc analysis, published in JAMA Ophthalmology, included a total of 1,009 participants who were originally enrolled in the Ocular Hypertension Treatment Study (OHTS) and followed from February 1994 to December 2008. The researchers created a glaucoma PRS using genome data from 8.8 million genetic variants from 449,186 individuals in the UK Biobank database. “As PRS is a relative measure within a population, we transformed our PRS to be centered at 0 with a standard deviation of 1 within the OHTS population, as recommended,” the team wrote in their journal article.
For analysis, they broke the range of PRS scores into 10 groups, or “deciles” as they’re called in statistics nomenclature. Among the OHTS participants, the mean PRS was significantly higher for 350 POAG converters (0.24) compared with 659 nonconverters (-0.12), and the risk increased by 1.36% with each higher PRS decile, with conversion ranging from 9.5% in the lowest PRS decile to 21.8% in the highest decile. In total, 212 participants (287 eyes) developed POAG.
The study authors also noted differences when PRS was stratified by ancestry. Mean PRS for 242 POAG converters of European descent was significantly higher than 519 corresponding nonconverters, and among those with African ancestry, mean PRS was not significantly higher for 140 POAG converters than for 108 nonconverters.
The authors believe this to be the largest genome-wide association study meta-analysis to date showing high POAG PRS is associated with increased risk for and earlier development of POAG conversion among patients with OHT. “This association was independent of most phenotypic baseline risk factors, genetically determined ancestry, and phase of OHTS follow-up period,” they wrote. “We also found that early IOP-lowering treatment may delay clinically detectable disease onset in those with high cumulative genetic risk. Lastly, the inclusion of a PRS improved multivariable risk stratification models.”
The fact that the study included 20 years of data from close follow up was one of the study’s strengths, say authors, however, potential misclassification of POAG in the UK Biobank codes or self-reporting is a limitation. “This is most likely to result in suboptimal training of the PRS and understate how well PRS predicts POAG. Furthermore, the relatively small size of the OHTS cohort, low proportion of participants with confirmed POAG, and loss to regular follow-up after 15 years likely limits the statistical power of our stratified comparisons and the predictive performance of our model,” they stated.1
This doesn’t diminish the substantial gains in understanding the link between PRSs and POAG, says a commentary published in the same issue of JAMA Ophthalmology. “The study’s key finding—that a PRS can independently predict the onset of POAG in individuals with ocular hypertension—is both groundbreaking and timely,” wrote the commentary author. “The study’s emphasis on genetic predisposition, as represented by PRS, adds a critical dimension to our understanding. By analyzing multiple genetic markers associated with POAG, PRSs provide a quantifiable risk assessment that complements traditional clinical evaluations. This approach may be particularly useful in patients with ocular hypertension, a known risk factor for POAG, potentially allowing for more nuanced risk stratification.”
The author further highlights the opportunity this research presents to advance personalized medicine for glaucoma, enabling optometrists and ophthalmologists to tailor monitoring and treatment strategies for patients with high PRS, while reducing the amount of surveillance on those with a lower PRS and potentially reducing health care costs for unnecessary interventions. The commentary author called for the development of PRS models that are inclusive of global genetic diversity, and concluded: “Continued research in this field is crucial to realize the full potential of PRSs in glaucoma management. By integrating genetic insights with clinical expertise, we may hope to substantially improve outcomes for individuals at risk of this sight-threatening disease.”2
1. Singh RK, Zhao Y, Elze T, et al. Polygenic risk scores for glaucoma onset in the Ocular Hypertension Treatment Study. JAMA Ophthalmol. March 14, 2024. [Epub ahead of print]. 2. Li F, Zhang X. The role of polygenic risk scores in glaucoma management. JAMA Ophthalmol. March 14, 2024. [Epub ahead of print]. |


