 |
|
Young adults may benefit most from genetic testing indicating risk for keratoconus, especially due to refractive surgery. Photo: Christine Sindt, OD. Click image to enlarge. |
Researchers have long known that a host of genetic factors can predispose patients to many ocular conditions, most notably inherited retinal disorders like achromatopsia, Leber’s, RP and Stargardt’s. Studies have also shown, more tenuously, a range of potential genetic influences on AMD, glaucoma and keratoconus. Efforts to create in-office tests for those latter examples that hold clinical value to optometrists and ophthalmologists, however, have struggled to establish a use case that leads to widespread adoption.
A study published in American Journal of Ophthalmology on May 11 added to the literature on the genetic underpinnings of keratoconus and researchers’ efforts to devise a multi-trait polygenic risk score (PRS) with predictive value. Four days later, Avellino Labs notified customers that it was discontinuing its AvaGen test marketed with this premise in mind.
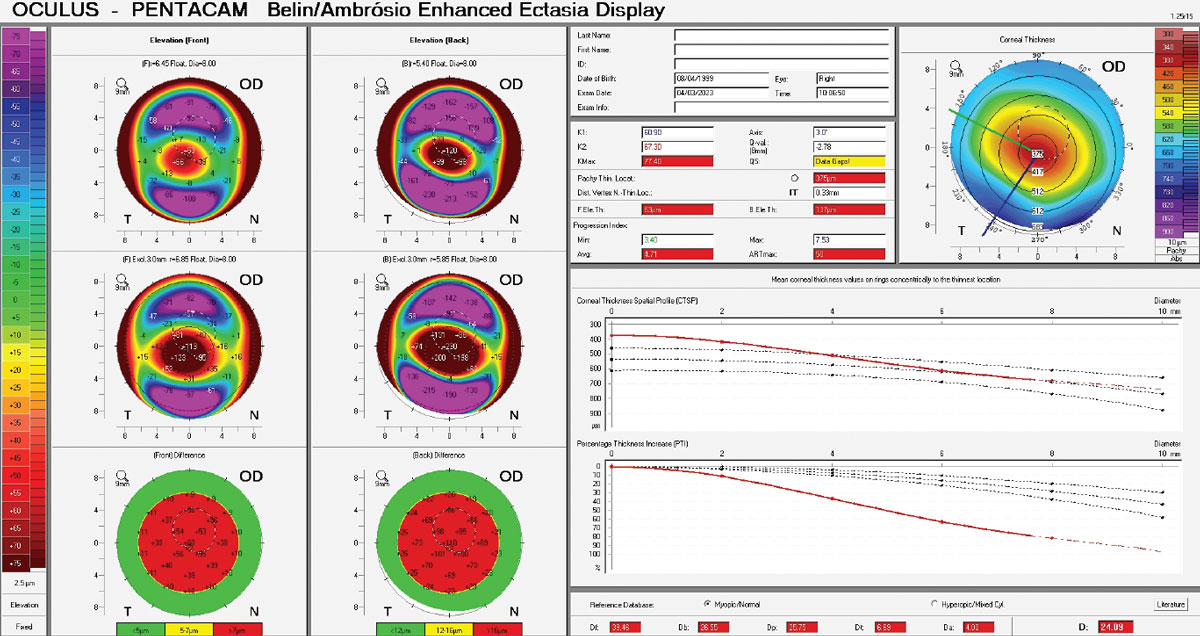
The AJO study included a total of 1,478 community-based young adults aged 18 to 30 from a single center. Of these, 609 returned for an eight-year follow-up. Scheimpflug imaging was conducted and subjects were genotyped, then a previously validated PRS was applied. Analyzed against the PRS as outcome measures were Belin/Ambrosio enhanced ectasia display (BAD-D) score and the presence of keratoconus, defined as BAD-D ≥2.6.
The study researchers found keratoconus prevalence to be 2.5% in this cohort. Each incremental increase in PRS was associated with a worse BAD-D and a 1.6x increased odds of keratoconus. Those who were in the highest PRS decile were more likely to have incident keratoconus in the third decade of life compared with the rest of the cohort. With each PRS increase, eight-year change in BAD-D score worsened.
From these observations, the authors list two potential important clinical implications for the setting of the PRS. “First,” they wrote in their paper, “genetic testing could be used as a tool to screen for those at risk of corneal ectasia prior to undergoing refractive surgery.” They equate this fact to the current rise of myopia prevalence, especially in younger generations. Consequently, they reason that more young adults will be undergoing laser refractive surgery, and, thus, this will result in an increased number of those who experience post-refractive ectasia.
The researchers note that ectasia induced by refractive surgery is preventable and adds to both patient morbidity and increased workload in the eyecare sector. As such, the authors believe that the PRS may help younger adults: “For people in this age group, it may be worth avoiding laser refractive surgery in those with high genetic predisposition to keratoconus.”
As another possibility, they propose that “a second utility of genetic testing is the prediction of keratoconus progression.” The authors stress that the condition typically stabilizes naturally around the fourth decade of life with varying degrees of severity seen. As such, it is critical to identify rapid progressors as well as those experiencing an older age at disease stabilization, since treatment methods, especially corneal crosslinking, is highly effective and cost-efficient in preventing progression and preserving vision.
Keratoconus progression is determined today through multiple corneal topography scans, with clinical evaluation of longitudinal changes. However, these changes observed over time can take several months up to a few years, affording the condition to progress further. “Genetic risk of keratoconus could provide an additional parameter with which the likelihood of further progression could be assessed,” the team concluded in their paper.
Commenting on the discordance between the promising research and lackluster clinical track record of keratoconus PRS tests, San Diego’s Brian Chou, OD, who cares for a large keratoconus patient base, says, “I believe the market failure of AvaGen was due to the lack of credibility. The concept was good, but the results did not demonstrate compelling predictive value, even for known keratoconus patients.” He adds that he hopes the experience “does not poison the well” for future attempts to launch such tests. “As this AJO article supports, there is value in genomics with keratoconus.” Dr. Chou mentions that good research on the genetics of keratoconus was conducted by Yaron Rabinowitz, MD, who passed away last November. Others will surely take up the mantle.
Lee SSY, Diaz-Torres S, He W, et al. Polygenic prediction of keratoconus and its measures: cross-sectional and longitudinal analyses in community-based young adults. Am J Ophthalmol. 2024:S0002-9394(24)00211-3. |


