A recent analysis seeking to better understand how social determinants of health (SDOH) impact the quality of diabetic eye care found that several factors influenced the degree to which patients received eye care in alignment with clinical practice guidelines. This research, published in the journal JAMA Ophthalmology, underscores the need for targeted interventions to improve outcomes for specific high-risk groups.
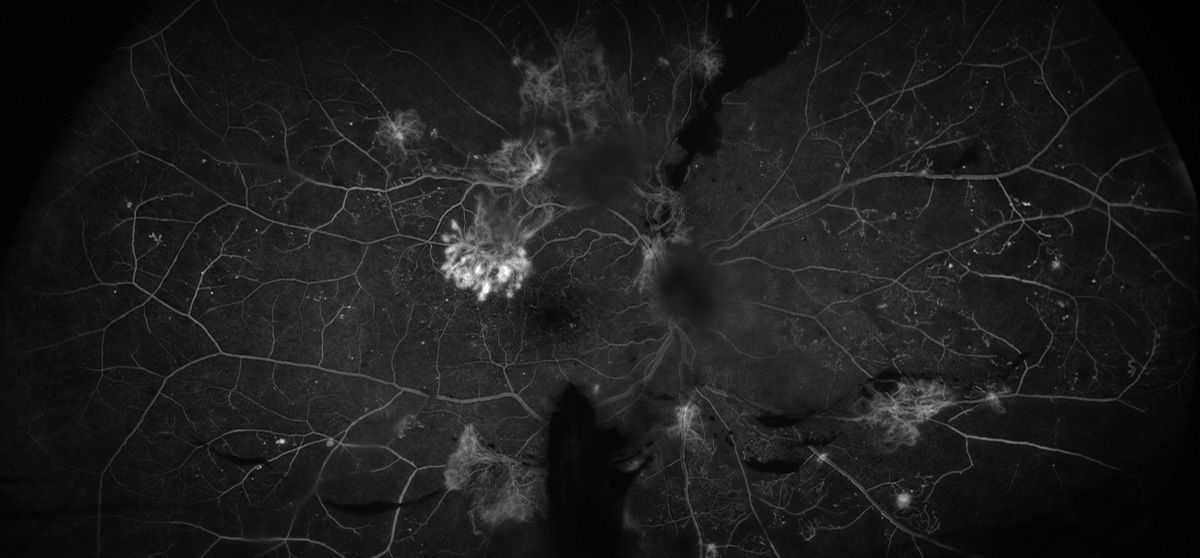 |
| This study underscores the need for focused strategies to address socioeconomic gaps in access to care for those with diabetic retinopathy. Photo: Rami Aboumourad, OD. Click image to enlarge. |
Conducted at 11 US medical centers, this cohort study included 37,397 adult patients (18 to 75 years old) with diabetes. Of those, 10,157 were Black and 27,240 were white. Study participants received care from 2012 to 2023 and had 18 months or more of follow-up.
When compared to those of the same race in urban communities, data showed that Black and white patients with diabetes who live in rural areas had 88% and 25% lower odds of having eye care visits, respectively. Comorbidities weren’t a factor, as sicker patients (defined by the Charlson Comorbidity Index) had 4% and 5% higher odds of having an eye care visit, respectively.
“Black patients with preexisting diabetic retinopathy (DR) had 15% lower odds of visits compared with those without preexisting DR while white patients with preexisting diabetic retinopathy had 16% higher odds of eye care visits,” the researchers noted in their recent JAMA Ophthalmology paper. Among patients who did receive eye care, those with preexisting diabetic retinopathy were more likely to receive dilated fundus exams.
In terms of health insurance, the investigation revealed that white patients with Medicare and Medicaid had lower odds of eye care visits when compared to their counterparts with commercial health insurance.
Hispanic patients were 15% less likely to have eye care visits compared to non-Hispanic white patients. Additionally, white patients with type 1 diabetes were 17% less likely to attend eye care visits than those with type 2 diabetes.
This study found that approximately half of patients with diabetes were undergoing DR monitoring that conformed to clinical practice guidelines, according to the study authors, who noted that while this research represents a small portion of the overall population of Black and white patients with diabetes, it demonstrates that some SDOH were associated with the likelihood of eye care visits.
“Among patients who received eye care, a majority underwent dilated fundus examinations for DR monitoring. We identified some racial similarities and some differences for particular SDOH associated with eye care visits,” the researchers concluded in their paper. “Of note, rural patients, white Hispanic patients and Black patients with preexisting DR tended to lack clinical practice guideline–recommended eye care, which may contribute to worse outcomes. These findings support exploring targeted interventions to improve care quality for these groups.”
An invited commentary on this study, also published in JAMA Ophthalmology, delved into the implications of this research as well as the importance of addressing disparities among patients with diabetes.
“Finding a solution to address the disparity in persons with diabetes will involve a multidisciplinary team approach to ensure that diabetic retinopathy screening standards are purposed for all persons with diabetes,” the commentators wrote. “The role of language barriers in patient care including instructions should be emphasized in future studies in addition to doing subgroup analysis on the Black patients with preexisting diabetic retinopathy to see what factors contributed to their decreased follow-up.
The study was well designed and demonstrates disparities in eye care among people with diabetes from different backgrounds, they noted. “Replication and further understanding of these observations could aid the ophthalmic community and policymakers as they design interventions to improve eye care.”
Chaudhury AS, Ige M, Marwah S, et al. Race, Social Determinants of Health, and the Quality of Diabetic Eye Care. JAMA Ophthalmol. September 12, 2024 [Epub ahead of print]. Movahedan A, Wroblewski KJ. Socioeconomic Determinants in Diabetic Retinopathy Screening. JAMA Ophthalmol. September 12, 2024 [Epub ahead of print]. |


