 |
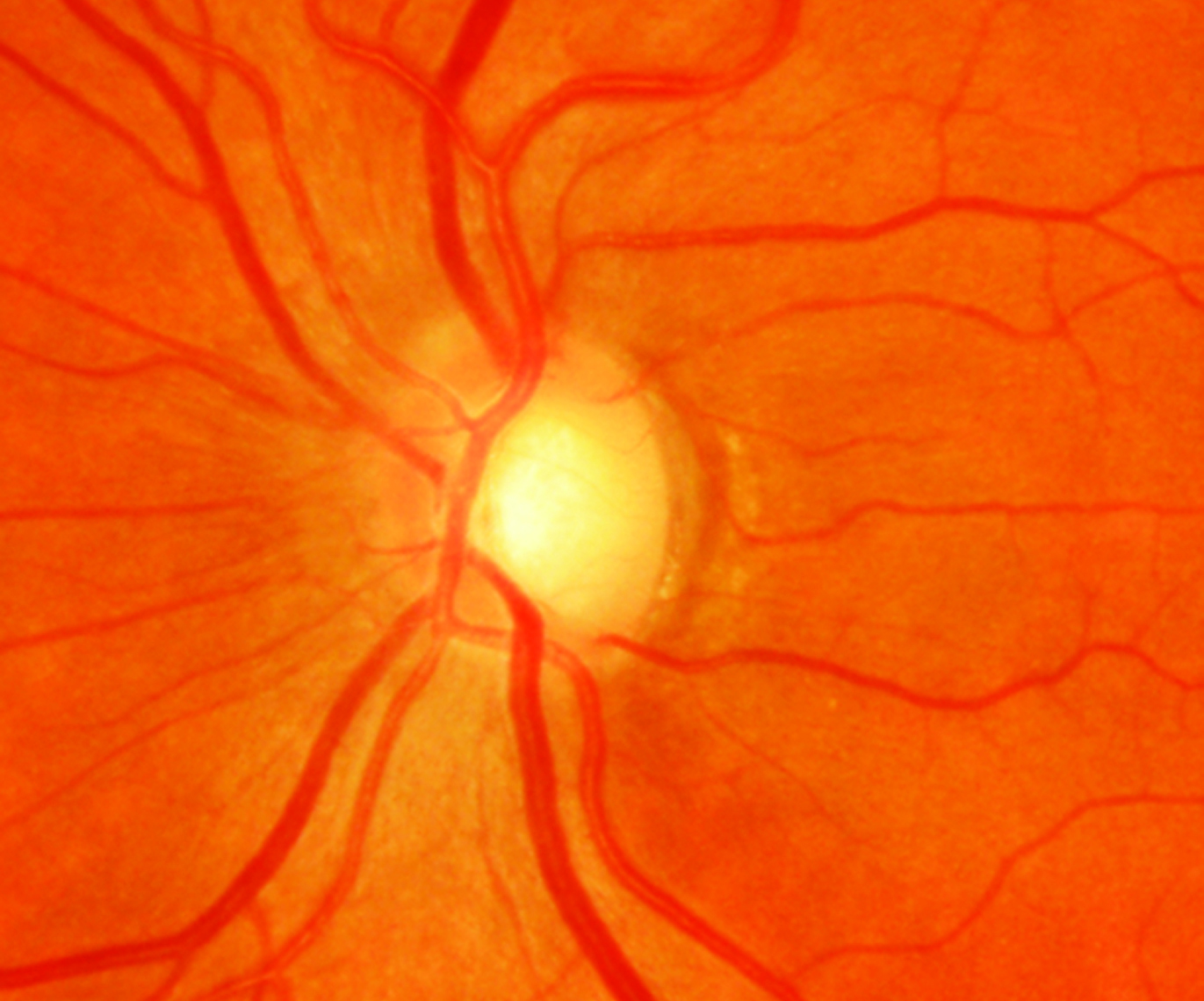
| Individuals in the high polygenic risk group, who also had known clinical risk factors, faced the highest risk of developing POAG. However, they also stood to benefit the most from early treatment, potentially mitigating the effect of genetic risk. Click image to enlarge. |
As technology advances and genetic testing becomes more accessible, the concept of a polygenic risk score (PRS) emerges as a promising tool for tailoring treatments to individual patients, potentially leading to improved outcomes. PRS analysis also presents an opportunity to identify those at low risk of disease in whom treatment or even increased surveillance may be unnecessary. Notably, this type of testing has also been shown to enhance the negative predictive power of thyroid, breast and lung cancer risk prediction.
Back in March of this year, JAMA Ophthalmology published the findings of a research team that determined PRS can independently predict the onset of primary open-angle glaucoma (POAG) in individuals with ocular hypertension. Last week, the journal published the group’s latest study regarding PRS. The team determined that a POAG PRS threshold can be used to identify individuals who are at low risk of disease onset, with those below the 48th percentile PRS threshold showing lower conversion rates over 20 years.
“While genetic risk for disease has some basis in ocular risk factors included in the baseline OHTS risk calculator (e.g., IOP, central corneal thickness, and cup-disc ratio), our findings show that a PRS may provide additional risk stratification to more accurately predict disease,” the researchers wrote in their paper.
To help differentiate patients at risk of glaucoma from those unlikely to develop vision loss, the Ocular Hypertension Treatment Study (OHTS) study identified five demographic and clinical factors predictive of POAG conversion. This predictive model, based on five-year data, performed well through 20 years, and these parameters have allowed for risk stratification among patients with ocular hypertension. This study was a post hoc analysis of the OHTS that included 1,010 individuals. Among the participants in this study, 65.8% were female, and the mean age was 55.9 years.
A mixed-effects logistic regression model adjusted for OHTS risk factors for conversion to POAG and randomization status determined that a PRS under the 48th percentile was associated with a 1.49 times higher likelihood of disease-free status after 20 years of follow-up (unadjusted hazard ratio: 1.64), compared with high polygenic risk.
Individuals below and above the POAG PRS threshold shared a similar distribution of baseline OHTS clinical risk, but those below the genetic risk threshold had more than twice the odds of remaining disease-free at 20 years.
After stratifying the trial cohort into nongenetic OHTS clinical risk tertiles, the largest differences in survival probability at 20 years based on PRS threshold were observed in eyes in the highest tertile of the initial observation group (20-year conversion rate: 61.1% in the high polygenic risk group vs. 23.8% in the low polygenic risk group), with randomization to early treatment partially mitigating the effect of high genetic risk (20-year conversion rate: 37.3% in the high polygenic risk group vs. 24.1% in the low polygenic risk group).
“Among those considered at highest risk based on the OHTS baseline model, early treatment may partially offset the effect of high genetic risk, but the benefit was limited for those with low genetic risk,” the researchers noted.
The team also suggested that “it is conceivable that a PRS-based POAG risk stratification approach could optimize the use of medical resources and effectively reduce costs.”
| Click here for journal source. |
Sekimitsu S, Ghazal N, Aziz K, et al. Primary open-angle glaucoma polygenic risk score and risk of disease onset: a post hoc analysis of a randomized clinical trial. JAMA Ophthalmol. November 7, 2024. [Epub ahead of print]. |


