A multitude of factors conspire to create disparities in ocular and visual health within the United States population and the world at large. In a new study for the purposes of public health education, researchers aimed to identify the characteristics and potential risk factors that are associated with higher rates of visual impairment in the US.
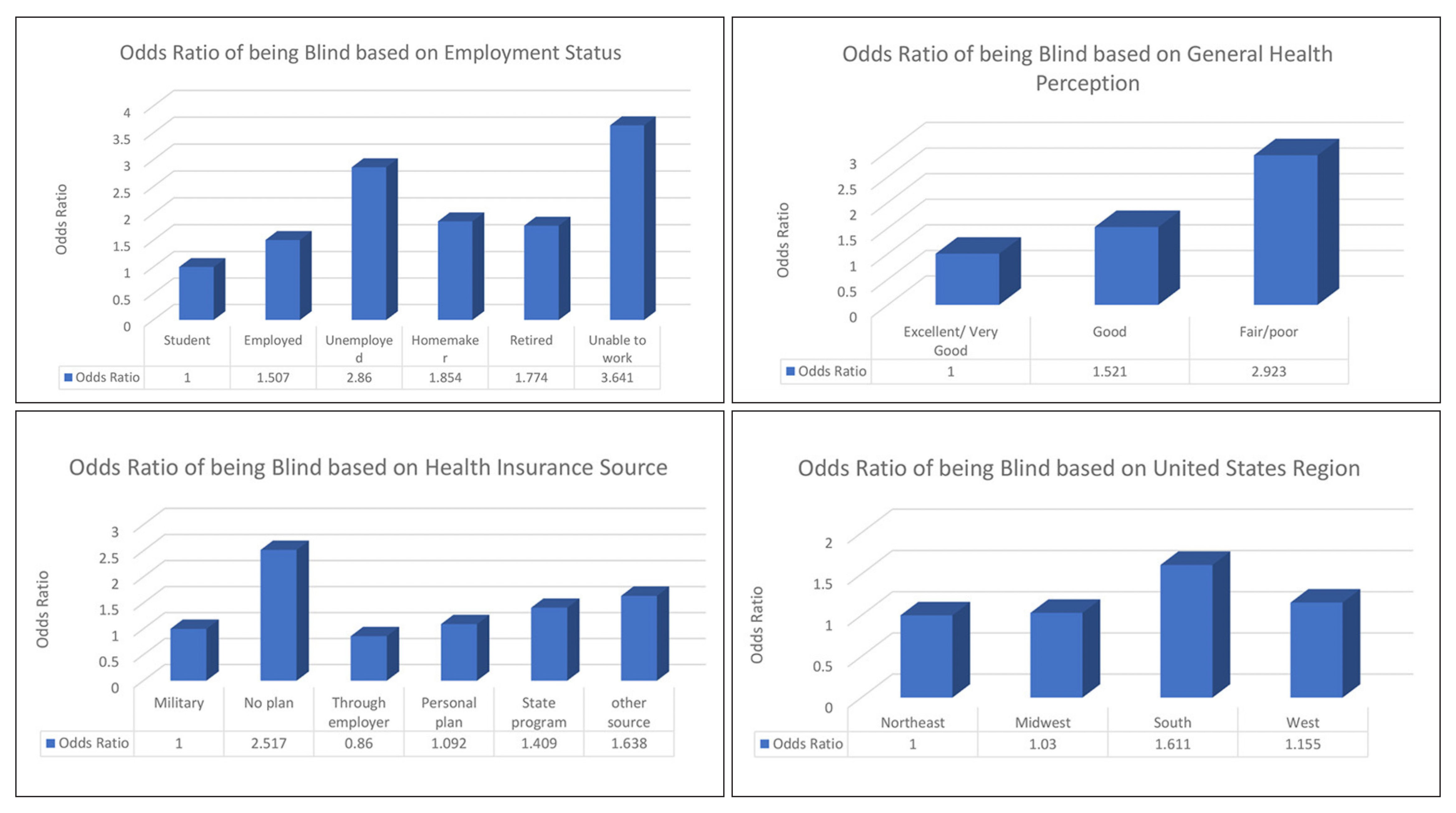
Data was obtained from the Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System from 2018 to 2021. Geographic location, perceived health status, employment status, income status, source of health insurance and age of the individual were associated with blindness or having serious difficulties seeing. Specifically, those who live in Southern states, with no insurance, have an income level below poverty and are of retirement age have the highest odds of suffering from visual impairment.
 |
|
|
“The factors listed above have an association with blindness or having serious difficulty seeing based on their odds ratio,” the researchers explained in their paper for Frontiers in Public Health. “We must study these factors further to learn the exact causal pathways that can influence whether a person becomes blind or has serious difficulty seeing so that we can reduce the number of people who suffer from visual impairment.” These factors, the authors argue, can guide development of interventions “by ensuring that the individuals in risk groups are targeted along with the rest of the population.” The odds ratios show that certain groups are at a higher risk of visual impairment due to socioeconomic, biologic or demographic factors, among others.
Finding ways to create better treatment options and make follow-up care accessible for those with visual impairment is needed, the authors emphasized, especially in the early stages to reduce the severity of vision loss. They suggest a holistic approach—comprehensive eye care—that encompasses treatment, prevention, promotion and rehabilitation for blindness, as a way to decrease the number of people who are diagnosed with an eye disease causing blindness or progressive vision loss.
“To this end, we need to educate patients and physicians on the comorbidities, groups who have higher chances of developing eye diseases, and available interventions depending on the disease such as cataract surgery, corrective lenses and anti-VEGF therapy, which have been shown to improve the quality of life for 150 million people worldwide,” the researchers explained in their paper. “To implement these interventions, we must encourage people to undergo annual screenings regardless of whether or not experiencing visual changes.”
The authors argue that more financial support should be allocated to education to help create a “more preventative initiative,” such as pop-up clinics, to allow minorities and those in the low socioeconomic status to obtain free and easily accessible eye screenings, which could decrease the rate of vision loss.
“It is critical to prevent the occurrence of diseases that can impact eye health by ensuring that all social groups are equally educated about them. This can be one of the only ways to truly decrease the number of people who lose vision due to health issues that could have been prevented by increasing the level of health literacy,” they explained.
Health literacy includes competence at absorbing both written and printed information as well as and numeracy (the ability to comprehend statistical data), and the authors noted that information should be available in multiple forms to reach every person in a way that can be informative.
“For example, a blind individual cannot read information unless it is Braille, so they must be able to listen to it, or someone who is deaf needs to be able to read the information,” the authors explained in their article. “In the US, 76% of adults have an education level less than a high school degree and 59% of older adults (65 years and older) are below or at the base level. We must make efforts to reach all individuals so there are no disparities in health education based on race, education level, age and geographic location.”
Future studies should delve more in depth into how medical costs, education status and body mass index vary among at-risk populations based on different levels, the authors suggested. “Another important direction is investigating the coverage provided by the main insurance companies regarding eye care in terms of examinations, procedures, medications, regulations and deductibles. This study showed that patients using government insurance have a greater chance of blindness than those who have private insurance.”
Powers AM, Patel D, DeAngelis MM, et al. Risk factors affecting the utilization of eye care services evaluated by the CDC’s behavior risk factor surveillance system from 2018 to 2021. Front. Public Health. June 10, 2024. [Epub ahead of print.] |


