 |
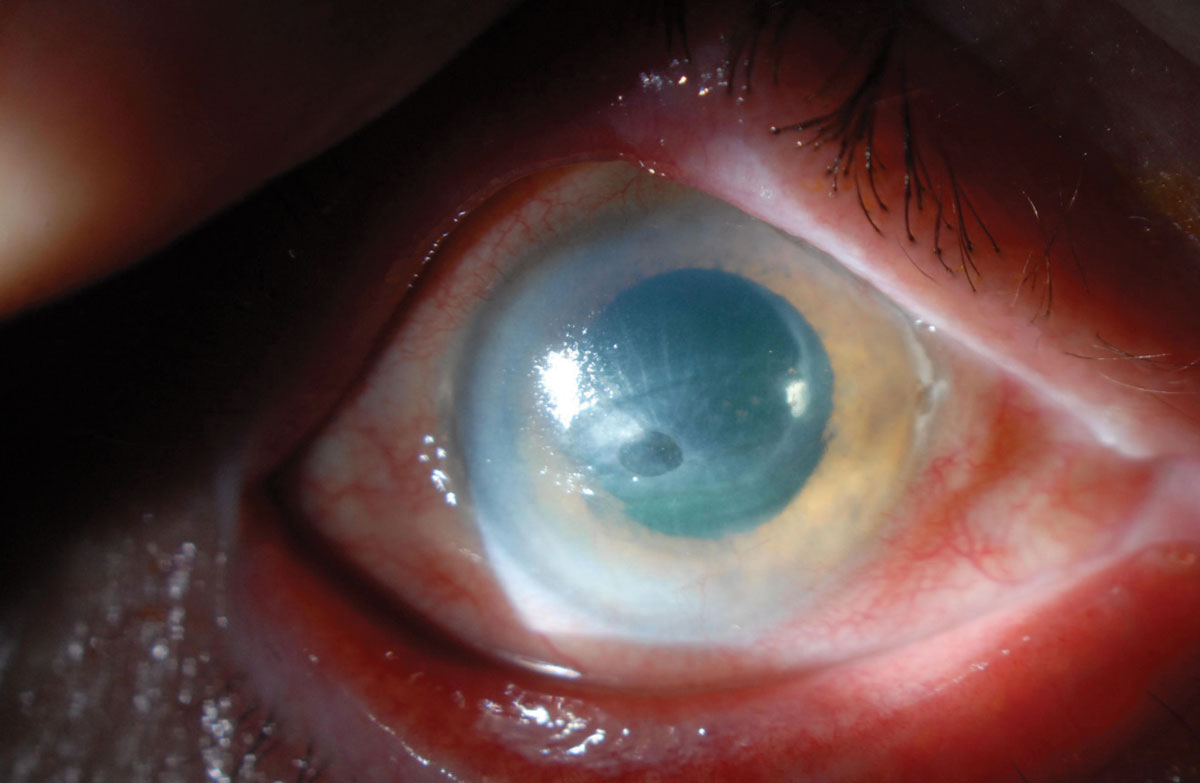
| A non-healing corneal ulcer in an eye with a history of herpes zoster ophthalmicus. The radial striae indicate significant corneal thinning. Photo: Christopher J. Rapuano, MD. Click image to enlarge. |
Previous studies have shown decreased corneal sensation—which can lead to neurotrophic keratopathy (NK)—in as many as 20% of patients with herpes zoster ophthalmicus (HZO), but little is known about the associated risk factors. In an effort to investigate this, researchers recently evaluated data from 896 patients who were seen over 10 years, with a median follow-up of 6.3 years.
NK developed in 6.5% of patients (n=58), with the highest hazard one to two years after onset of HZO. Age, Caucasian ethnicity, best-corrected visual acuity (BCVA), intraocular pressure, corneal involvement, uveitis and number of recurrences were associated with increased risk of NK. The association of recurrences with NK suggests the possibility of ongoing nerve damage during these episodes. Additionally, vision loss was about 66.7% more frequent in those with NK.
Corneal involvement was associated with NK on univariate, but not multivariate, analysis. The authors noted that this is likely because many patients did not have corneal involvement on the initial presentation but later developed it.
“Because BCVA at initial presentation was associated with NK, it is also possible that patients may have had subtle corneal findings that were missed initially,” they explained.
No association of NK occurrence with either prompt antiviral treatment (within 72 hours) or treatment duration was identified. “However, there was little variation in the duration of treatment, with most having received treatment for seven days, which would have limited the ability to detect any effects of antiviral duration on NK occurrence,” the authors noted.
The risk factors presented here may necessitate surgical procedures to stabilize the ocular surface, which can progress to loss of vision despite interventions, they concluded.
Meyer JJ, Liu K, McGhee CNJ, et al. Neurotrophic keratopathy after herpes zoster ophthalmicus. Cornea. December 26, 2021. [Epub ahead of print]. |


