 |
|
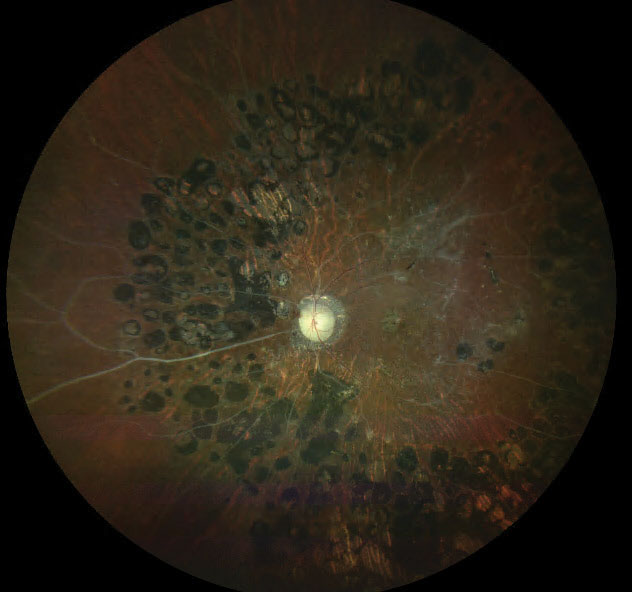
Policies aimed at improving living conditions and participation of people with vision difficulties in the community might result in improved access to healthcare, spanning access to food, housing, transportation and employment. Photo: Erin Kenny, OD, and Christin DeMoss, OD. Click image to enlarge. |
An aging US population is projected to lead to a rise in the prevalence of vision loss, which underscores the critical need to address existing disparities in healthcare access for adults experiencing vision difficulties. Researchers at the Johns Hopkins Disability Health Research Center in Baltimore recently offered an update on national-level estimates of healthcare access for individuals with disabilities in a paper for Ophthalmic Epidemiology. They found that American adults who report visual difficulties were more likely to face challenges accessing care than those without. These disparities around having health insurance coverage, a usual healthcare provider, regular health check-ups and affording care highlighted areas to target efforts from a public health policy perspective.
The study used data on 1,258,919 participants surveyed from the 2019, 2020 and 2021 cycles of the Behavioral Risk Factor Surveillance System (BRFSS), a national telephone-based survey of US adults 18 years old and older conducted by the US Centers for Disease Control and Prevention.
Participants who responded yes to the question “Are you blind or do you have serious difficulty seeing, even when wearing glasses?” were considered to have vision difficulties. Of all subjects, 5.1% reported having these difficulties.
As compared to adults without vision difficulties, adults who reported difficulties were older (≥65 years; 31.9% vs. 21.5%) and more likely to be female (56.3% vs. 50.7%). These adults were also more likely to have less than a high school education (27.3% vs. 11.5%), a household income of < $25,000 USD (51.5% vs. 21.5%) and be unemployed (44.5% vs. 23.5%) than adults without vision difficulties. Multivariable regression analyses showed that adults with vision difficulties reported greater odds of having no coverage (odds ratio; OR = 1.14), having no provider (OR = 1.12), having a health checkup less than one year ago (OR = 1.12) and being unable to afford care (OR = 1.62), as compared to adults without vision difficulties. In sensitivity analysis restricted to adults >65 years, the results for having no healthcare coverage were similar with those found in the full population (OR = 1.12).
“Policies aimed at strengthening provisions around accessibility of healthcare facilities might result in increased access to healthcare for this population,” the researchers concluded in their paper. “Improving accessibility of facilities and communication is key to building healthcare systems that are more hospitable to people with low vision.”
| Click here for journal source. |
Onukwugha C, Castro F, Swenor BK, Varadaraj V. Disparities in healthcare access for adults with self-reported vision difficulty - Behavioral Risk Factor Surveillance System 2019–2021. Ophthalmic Epidemiol. November 12, 2024. [Epub ahead of print]. |


