 |
It’s been said, “You can easily do any job as long as you have the right tool.” Optometrists may overlook valuable tools at their disposal to provide premium care to patients. The following discussion gives an overview of several of the newest ocular surface–based instruments and what you may need to implement them in your practice.
 |
|
Meivertor grasping the lashes to evert the eyelid. Click image to enlarge. |
Eyelid Everters
One of the more exciting new instruments is the Meivertor. Its disposable silicone tips gently grasp lashes with a simple turning motion and the eyelid is everted. The advantage is that it frees the other hand. Additionally, it can also keep the everted eyelid in place longer for procedures such as concretion or inclusion cyst removal. It’s easier on you and the patient for a quick upper eyelid assessment during a routine exam or to identify a potential foreign body. Gone are the days of having difficulty everting an eyelid or missing a subtle foreign body. Additionally, if you offer meibography, you have a tool that staff can easily use to effectively capture the image without the need for a second technician to hold the eyelid.
 |
|
The smooth rounded tip and diamond dust on the forceps prevent epithelial cell damage when removing a BCL. Click image to enlarge. |
Forceps
These include toothed and non-toothed styles. Toothed instruments allow for greater control during procedures rather than conventional forceps or hands. With greater control, you are able to provide efficient and effective care to patients in comparison to conventional means. Newer instruments also allow for smooth edges and tips, removing the potential for insult to the ocular surface. These provide added comfort for patients, potentially removing the need for anesthetics. Additionally, you are able to be more precise by staying within the slit lamp to administer treatment.
One unique instrument is a diamond dust covered, smooth-end forceps, which is employed in the removal of a bandage contact lens (BCL). The use of fingers to pinch a BCL can sometimes remove epithelium along with it—especially in the early healing course of an abrasion or recurrent corneal erosion—impart pathogens or cause injury. The BCL forceps break suction instantly by grasping the BCL at the temporal edge and removing it. Because the forceps have a smooth end, you can’t poke or injure the conjunctiva as you slide it under the BCL. Once it’s grasped, it is an easy removal and practically impossible to cause an abrasion.
 |
The grooves in these extended-duration punctal plug forceps allow for easy capture and insertion. Click image to enlarge. |
The removal of inclusion cysts is one instance where using toothed forceps instead of jeweler forceps would be a more effective and valuable treatment option. Traditionally, inclusion cysts are drained by puncturing the affected area with a large-gauge needle; however, this procedure yields high recurrence rates.
A more robust treatment option would be to use the toothed forceps to elevate the central portion of the cyst, allowing you to create an incision immediately below the area for an increased drainage zone. Jeweler’s forceps would not likely hold the cyst in the center and could pose a risk for injury by their sharp leading edge. The curved end of the toothed forceps allows you to grasp the cyst without worry of injury. Control of the conjunctiva throughout the procedure is maintained due to the inside toothed nature of the forceps as opposed to the smooth inside of jewelers.
 |
| Prokera forceps allow for easy removal of the remnant ring without the risk of trauma to the ocular surface. Click image to enlarge. |
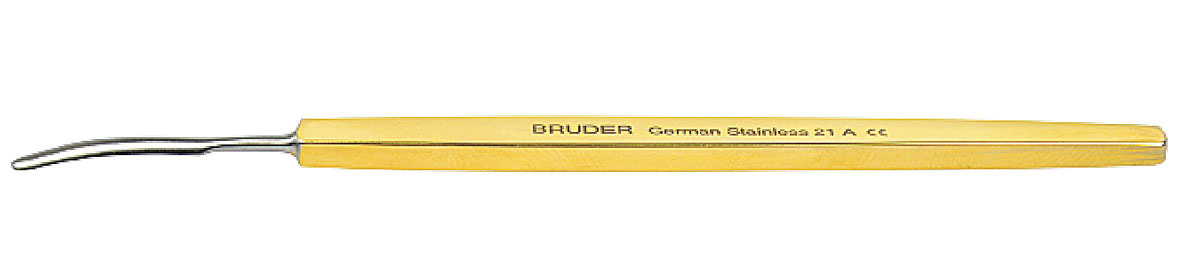
Insertion of punctal plugs can be accomplished through various means. Unless insertion is performed with a pre-loaded plug, forceps must be involved. In order to properly grip the plug, the doctor is required to have the punctal plug inside the forceps. Due to the smooth nature of regular jeweler’s forceps, a higher level of pressure must be applied when clamping the plug. This pressure can cause the punctal plug to be crushed or to fly off as it is squeezed. The sharp tip of jewelers may also increases risk of potential injury to the patient. Punctal plug forceps (Bruder) have a groove designed to fit these extended-duration plugs, which provides control of the plug while minimizing pressure. It also allows the plug to be nearly parallel with the forceps. Parallel angle insertion is less challenging than a traditional perpendicular angle, thus reducing stress for you and the patient.
The implementation of cryopreserved amniotic membranes is becoming commonplace in practices across the nation. Although insertion of the Prokera Lens Forceps is easily performed with one’s fingers, the removal of the ring post-treatment can be the challenge. The smooth leading edge allows you to easily grasp and maintain better control, which results in more comfort for the patient. When a patient experiences discomfort during removal, proper gaze may become unstable. Irregular fixation during removal can further lead to excess damage of the ocular surface, redacting the purpose of the amniotic membrane. Other methods such as fingertip removal or another type of forceps could be applied, but will not supply the necessary control and grasp needed to most efficiently and safely remove the amniotic membrane remnant. Because these forceps are rounded, you can’t injure the conjunctiva as you try to grasp the ring edge.
 |
| Dry Amnion Forceps (Bruder) allow for easy placement, protecting the membrane and preventing it from folding over. Click image to enlarge. |
The Apollo Amniotic Membrane (Atlas Ocular) forceps share a similar smooth-edge, which also provides better safety but also protects the delicate membrane and prevents it from folding. There are multiple ways to position a dehydrated amniotic membrane on the eye. A more sterile environment is maintained due to the forceps’ ability to grasp the membrane within its original packaging. Placement of the membrane is similar when using other forceps, due to the membrane having a high affinity to the ocular surface. The instrument’s design allows for the position of the membrane to be more precise and prevents compared to sharp-edge or pointed forceps.
 |
|
Lid debriders have been shown to improve MG function. Click image to enlarge. |
Debridement/Scaling
MGD Paddles/Expression Tools
It is essential to diagnostically express MGs. Although they can be expressed digitally, having an instrument is typically more effective. With the patient in the slit lamp, simply place a soft-edged paddle behind the lower eyelid and with your thumb on the outside, slide the paddle upward. You can readily see the expression and grade five MGs in the lower eyelid central region in about five seconds.
Instruments are essential to successful optometric practice and newer designs, especially in the area of ocular surface disease, are making practice safer, more effective and easier. It’s well worth incorporating many of these tools to enhance your practice, better perform procedures and elevate the care you provide.
1. Korb DR, Blackie CA. Debridement-scaling: a new procedure that increases Meibomian gland function and reduces dry eye symptoms. Cornea. 2013;32(12):1554-7. 2. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472-8. |

