 |
We’re in the early days of the rollout of Xdemvy (lotilaner ophthalmic solution 0.25% Tarsus), the first FDA-approved prescription medication for Demodex blepharitis, a condition that affects at least 25 million Americans.1 Despite its pervasive nature, Demodex blepharitis is an underdiagnosed disease, but fortunately with easy to identify pathognomonic clinical signs and a host of symptoms.
Let’s dive into this condition, what signs to look for and the new treatment poised to wipe out Demodex.
What is Demodex Blepharitis?
Demodex is the most common ectoparasite found in humans, with prevalence rates as high as 58% of all patients.1 It is also the cause of about seven out of 10 cases of blepharitis.1-3 The Demodex mite has two forms: Demodex folliculorum and Demodex brevis. The first, D. folliculorum, tends to involve the lashes and particularly within the lash follicle itself, while D. brevis affects the sebaceous glands of the skin, as well as the meibomian glands of the eyelid. D. brevis has been implicated as a contributor to ocular rosacea.4
Studies show that 59% of all patients presenting with facial rosacea have Demodex blepharitis.5 The condition occurs more often in contact lens wearers, with research showing that 90% are positive for Demodex blepharitis.6 Even more startling is the fact that 93% of contact lens–intolerant patients were positive for Demodex blepharitis.1
 |
|
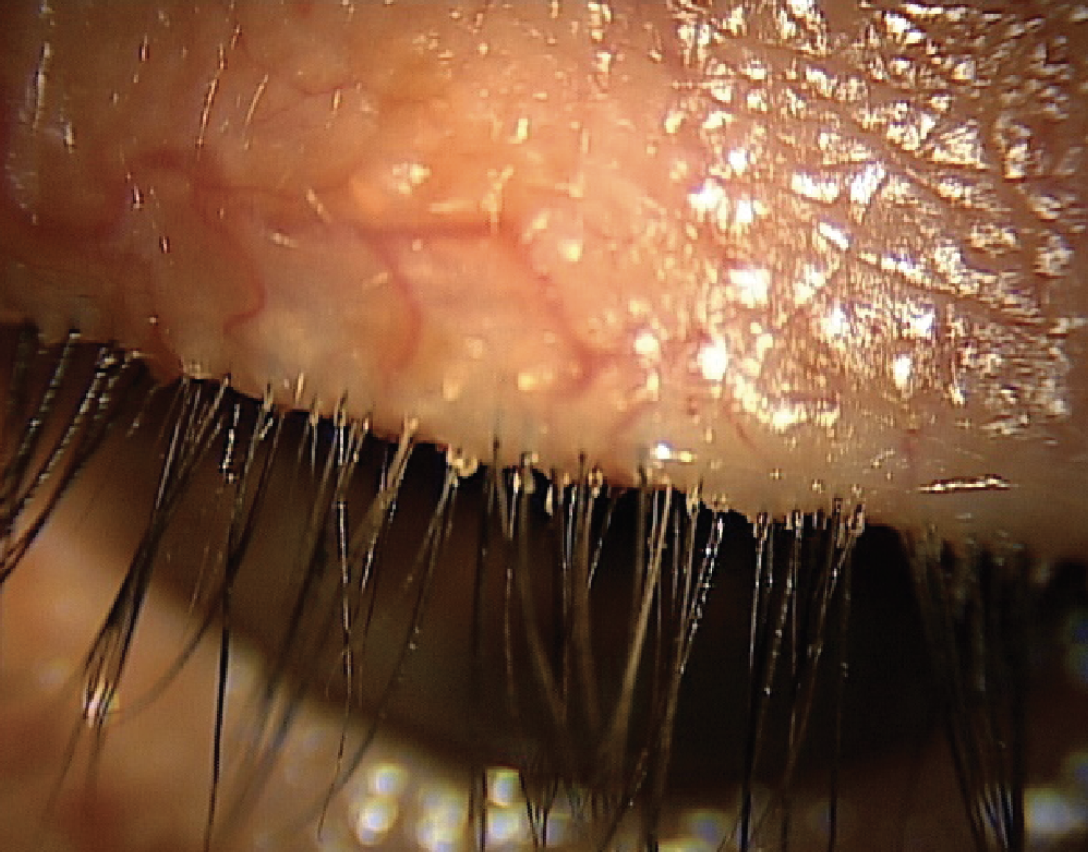
Debris at the base of the lashes is a hallmark sign of Demodex blepharitis. Click image to enlarge. |
Diagnosis
Collarettes, or a sleeve or debris at the base of the lashes, is the hallmark sign of Demodex blepharitis. They are composed of mite waste products, digestive enzymes and eggs, resulting in red, irritated and itchy eyelids.3 Patients might also experience dryness, grittiness and foreign body sensation. A clinician doesn’t require extra tools or equipment to make the diagnosis. Simply have the patient look down while at the slit lamp and increase the magnification, as it helps you scan the base of the upper lashes.
Because it affects the meibomian glands, Demodex can also be associated with meibomian gland dysfunction, frequent or recurring hordeola/chalazia and evaporative DED.3,8-9
Unique Properties
Lotilaner, the active ingredient in Xdemvy, has been used in veterinary medicine for the treatment of parasites in canines. Lotilaner is a non-competitive antagonist of parasitic gamma-aminobutyric acid–gated chloride channels; blocking these channels results in paralysis and death of the Demodex mite.
FDA Approval
In the pivotal FDA clinical trials of Xdemvy, efficacy and safety was met with 415 patients in the treatment arm, with significant reductions in collarettes and erythema improvement observed as early as two weeks and at the primary endpoint, day 43. The most common adverse event was burning upon instillation in about 10% of patients.
All Xdemvy therapy takes is one drop, twice a day over a six-week period. This covers the entire lifecycle of the mite and eggs and will ensure high levels of eradication as well as enhance our patients’ ocular health and quality of life.
Dr. Karpecki is the director of Cornea and External Disease for Kentucky Eye Institute, associate professor at KYCO and medical director for Dry Eye Institutes of Kentucky and Indiana. He is the Chief Clinical Editor for Review of Optometry and chairman of the affiliated New Technologies & Treatments conferences. A fixture in optometric clinical education, he provides consulting services to a wide array of ophthalmic clients. Dr. Karpecki’s full disclosure list can be found here.
1. Trattler W, Karpecki P, Rapoport Y, et al. The prevalence of Demodex blepharitis in US eye care clinic patients as determined by collarettes: a pathognomonic sign. Clin Ophthalmol. 2022;16:1153-64. 2. Zhang AC, Muntz A, Wang MTM, et al. Ocular Demodex: a systematic review of the clinical literature. Ophthalmic Physiol Opt. 2020;40(4):389-432. 3. Fromstein SR, Harthan JS, Jaymeni P, Optiz DL. Demodex blepharitis: clinical perspectives. Clin Optom (Auckl). 2018;10:57-63. 4. Forton FMN. Rosacea, an infectious disease: why rosacea with papulopustules should be considered a demodicosis: a narrative review. J Eur Acad Dermatol Venereol. 2022;36(7):987-1002. 5. Gonzalez-Hinojosa D, Jaime-Villalonga A, Aguilar-Montes G, Lammoglia-Ordiales L. Demodex and rosacea: is there a relationship? Ind J Ophthalmol. 2018;66(1):36-8. 6. Jalbert I, Rejab S. Increased numbers of Demodex in contact lens wearers. Optom Vis Sci. 2015;92:671-8. 7. Tarkowski W, Moneta-Wielgos J, Mlocicki D. Demodex Sp. as a potential cause of the abandonment of soft contact lenses by their existing users. Biomed Res Int. 2015;2015:259109. 8. Liu J, Sheha H, Tseng, SCG Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505-10. 9. Cheng AM, Sheha H, Tseng SCG. Recent advances on ocular Demodex infestation. Curr Opin Ophthalmol. 2015;26(4):295-300. |

