 |
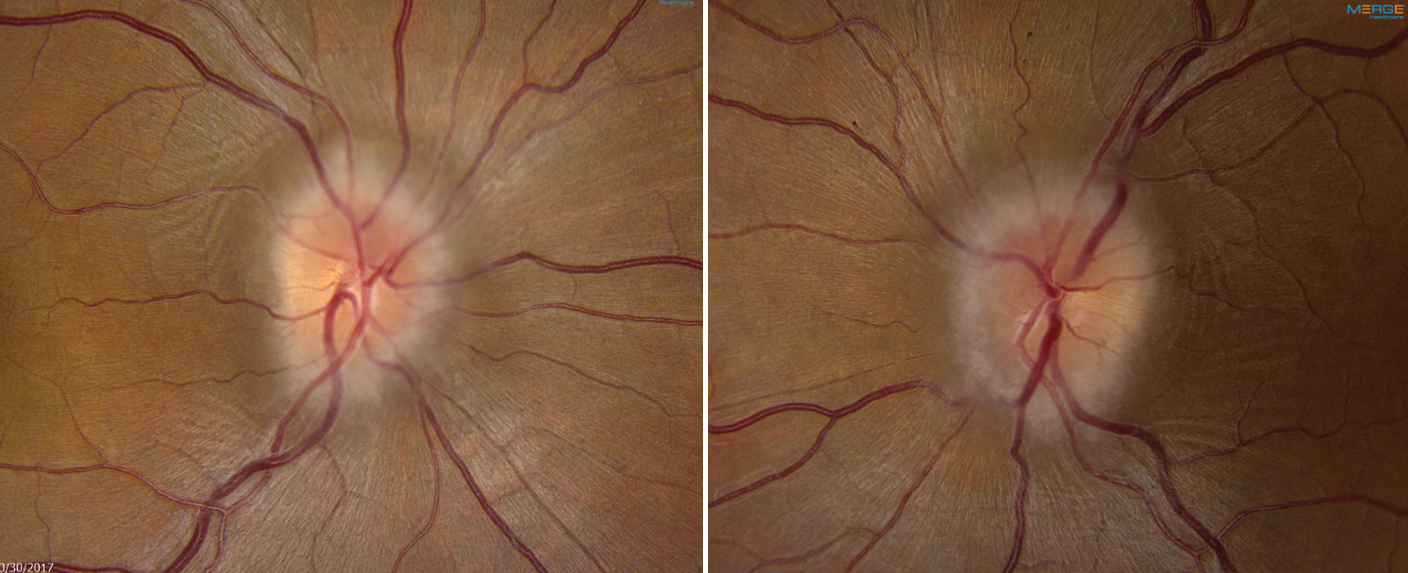
| Study suggests that those over 45 years old with IIH may represent milder chronic disease that was previously undiagnosed. Photo: Alison Bozung, OD. Click image to enlarge. |
Idiopathic intracranial hypertension (IIH) typically affects obese women of childbearing age, with numerous studies confirming these and other clinical characteristics. Although it’s somewhat rare for older patients to have this condition, it’s been reported that there may be some important differences. In a new study from Journal of Neuro-Ophthalmology, researchers investigated how this disease presents differently in these age groups and can help clinicians better understand how to diagnose and manage it.
A total of 167 patients diagnosed with IIH were divided into two groups: 135 subjects between 18 and 44 years old and 32 subjects age 45 or older.
The younger group had a higher rate of headaches (90% vs. 63%), higher body mass index (38.9 vs. 36.1), higher opening pressure (38cm H2O vs. 31cm H2O) and thicker peripapillary retinal nerve fiber layer average thickness (right eye 178mm vs. 131mm; left eye 184mm vs. 136mm).
On the other hand, the older group had higher rates of empty sella (90% vs. 62%). The 90% rate closely matches the overall prevalence of findings in patients with IIH in other studies (85%), the authors noted.
“In our study, both of these figures are higher than the rate of empty sella noted in the general population, which is 6% to 20%. This finding suggests a linear relationship, with the duration and severity of the disease having a positive correlation with the imaging findings,” the researchers explained in their paper for the journal.
“Future studies powered to compare age differences in this finding may offer further insights on whether empty sella increases with age, severity of disease and/or disease duration. Such future studies may also benefit from a more uniform and formal definition of what constitutes ‘empty sella,’ they wrote.
In addition, in the younger group, there was a trend toward higher rates of pulsatile tinnitus (63% vs. 45%), transient visual obscurations (50% vs. 32%)—suggesting more severe disease at presentation—and lower rates of spontaneous cerebrospinal fluid (CSF) leak (4% vs. 13%).
Previous studies have examined the prevalence of IIH in patients with CSF leaks; however, to the best of the authors’ knowledge, no studies have evaluated the reverse as in this study: the prevalence of CSF leaks in patients known to have IIH. “This is likely due to the low prevalence of spontaneous CSF leaks in patients with IIH and the fact that the presence of a leak confounds the diagnosis of the underlying IIH because of the subsequent spontaneous drop in CSF pressure,” the authors explained. “It is possible that the higher prevalence numbers seen in the older patients in our study may reflect the more chronic nature of the disease in the older cohort.”
Sex, rates of obesity, other MRI findings typical of elevated intracranial pressure, frequency and Frisen grading of papilledema, and visual field loss were not statistically different between the groups.
The report concludes that the older age group had milder signs and symptoms of IIH and a higher prevalence of empty sella than the younger group, but otherwise had typical characteristics. These findings suggest that IIH in the older age group may represent milder chronic disease that was previously undiagnosed.
Sabet SJ, Gasquet NC, Henderson AD, Carey AR. Clinical characteristics of idiopathic intracranial hypertension in older adults. Jour Neuro-Ophthamol. January 18, 2024. [Epub ahead of print.] |

