 |
A 52-year-old Nicaraguan male presented to the emergency department with a subjective blind spot in the temporal field of his left eye starting the day prior. He also observed floaters, photopsias and central blurred vision in the same eye. He denied any ocular trauma, pain or recent surgery. His medical history included hypertension and hypercholesteremia, both controlled with medications.
On examination, the patient’s visual acuity with pinhole was 20/25 in both eyes. His intraocular pressures, color vision and confrontation visual fields were normal. He did not have an afferent pupillary defect. The anterior segment exam was unremarkable in both eyes, but there were rare white blood cells in the vitreous cavity of the left eye. The fundus exam revealed moderate cup-to-disc ratios in both eyes with fine pigmentary changes in the left eye (Figure 1). Fundus photography, OCT and fundus autofluorescence (FAF) were obtained and revealed interesting findings (Figures 2 and 3). All imaging of the right eye was unremarkable.
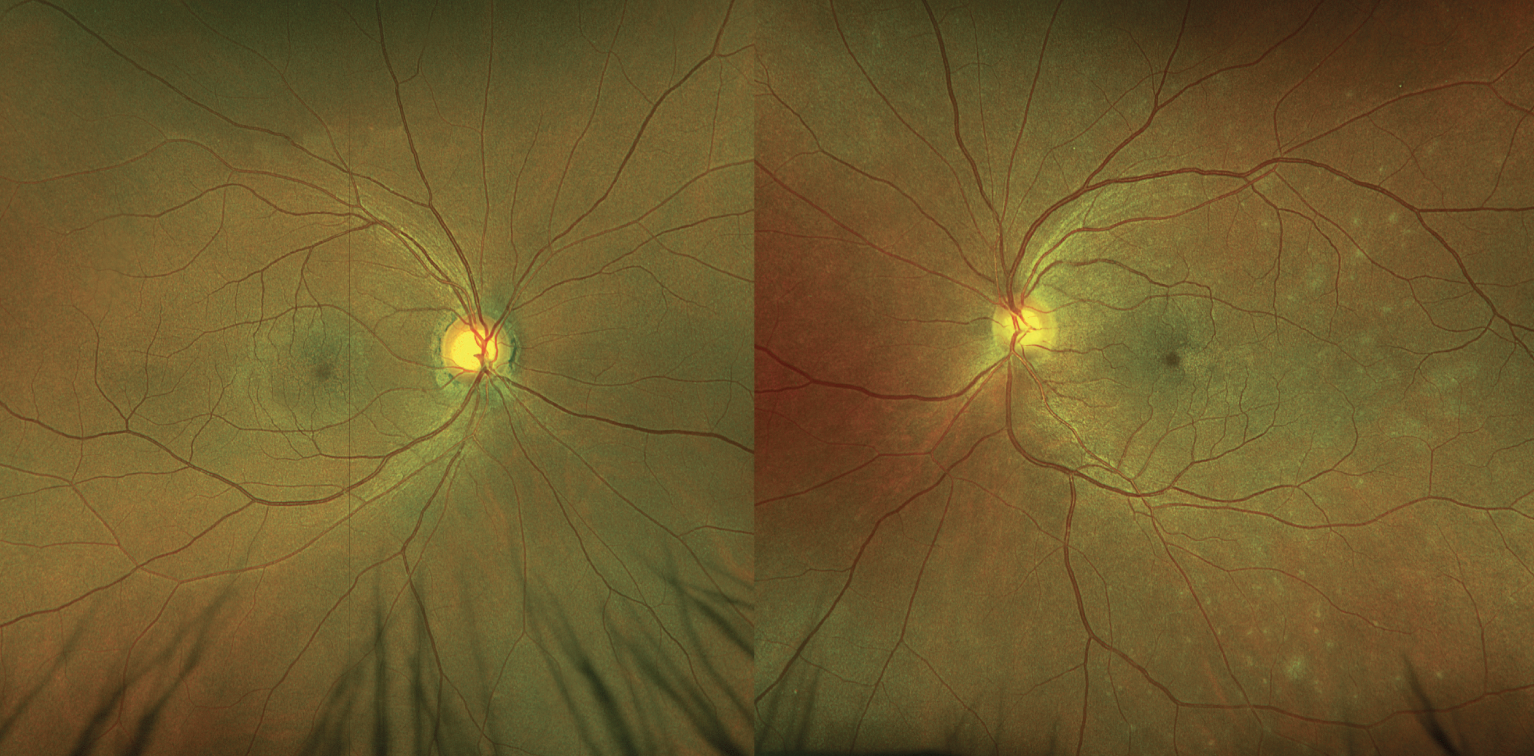 |
Fig. 1. Right and left fundus photos. The left fundus (right image) has subtle whitish granular lesions in the posterior pole. Click image to enlarge. |
Fundus findings prompted a more detailed case history, and the patient denied any recent viral infection symptoms, skin rashes, mucocutaneous ulcers, recent travel, non-productive cough or shortness of breath. He also denied any known history of bacterial infections, such as syphilis or tuberculosis.
Diagnosis
Based on the clinical vignette and imaging, a diagnosis of multiple evanescent white dot syndrome (MEWDS) was made. No medications were initiated, and the patient was instructed to return for short-interval follow-up. Laboratory testing was ordered at a follow-up visit to rule out syphilis and tuberculosis, which the patient ultimately chose not to receive. Three weeks after his initial presentation, the retinal lesions had begun resolving and his vision improved to 20/20. Presumably due to resolution of his symptoms, the patient did not return for his follow-up appointment.
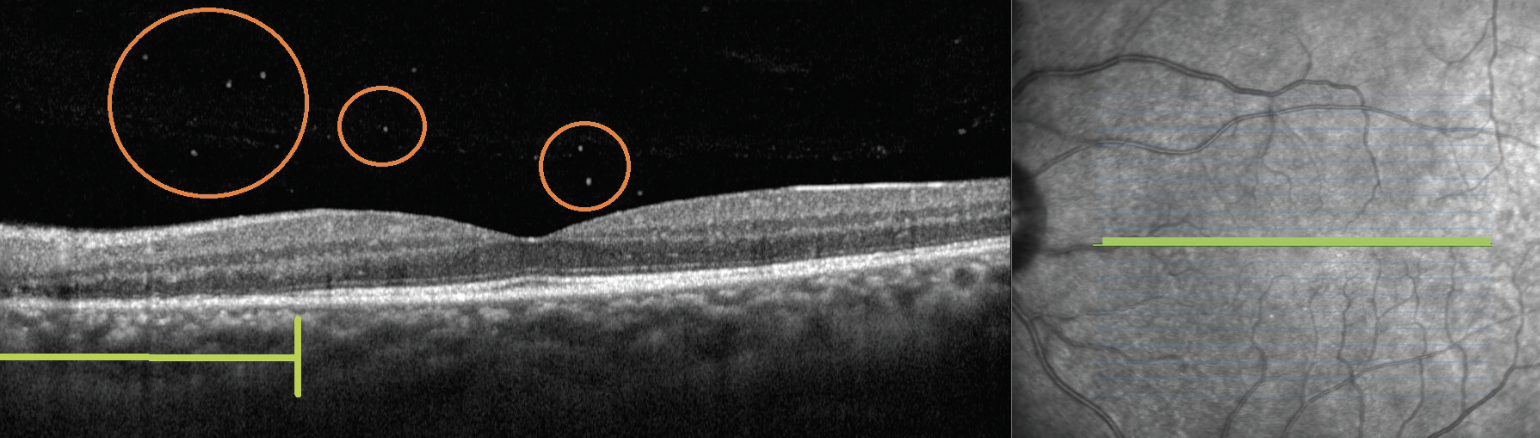 |
Fig. 2. OCT of the left eye, revealing outer retinal loss of the ellipsoid zone (denoted by underlying green bracket) and subtle vitreous cell (circled in orange). These findings were unilateral. Click image to enlarge. |
Presentation
MEWDS is often listed amongst the “white dot syndromes.” The inflammatory condition is unilateral in the majority of cases and is most common in the third to fourth decades of life. As with many posterior uveitis syndromes, it has a predilection for myopic women. About one-third to one-half of individuals with MEWDS experience a flu-like viral prodrome. Others have been diagnosed after receiving various vaccinations.1 Although the exact mechanism of disease is still unknown, an autoimmune, post-viral pathogenesis has been suggested.2 There may also be a genetic component, as the HLA-B51 haplotype has been implicated.3 The exact location of the pathologic process is contested, with some stating the choriocapillaris is the primary location of insult and others claiming the outer retina and photoreceptors are predominantly impacted.1,4,5
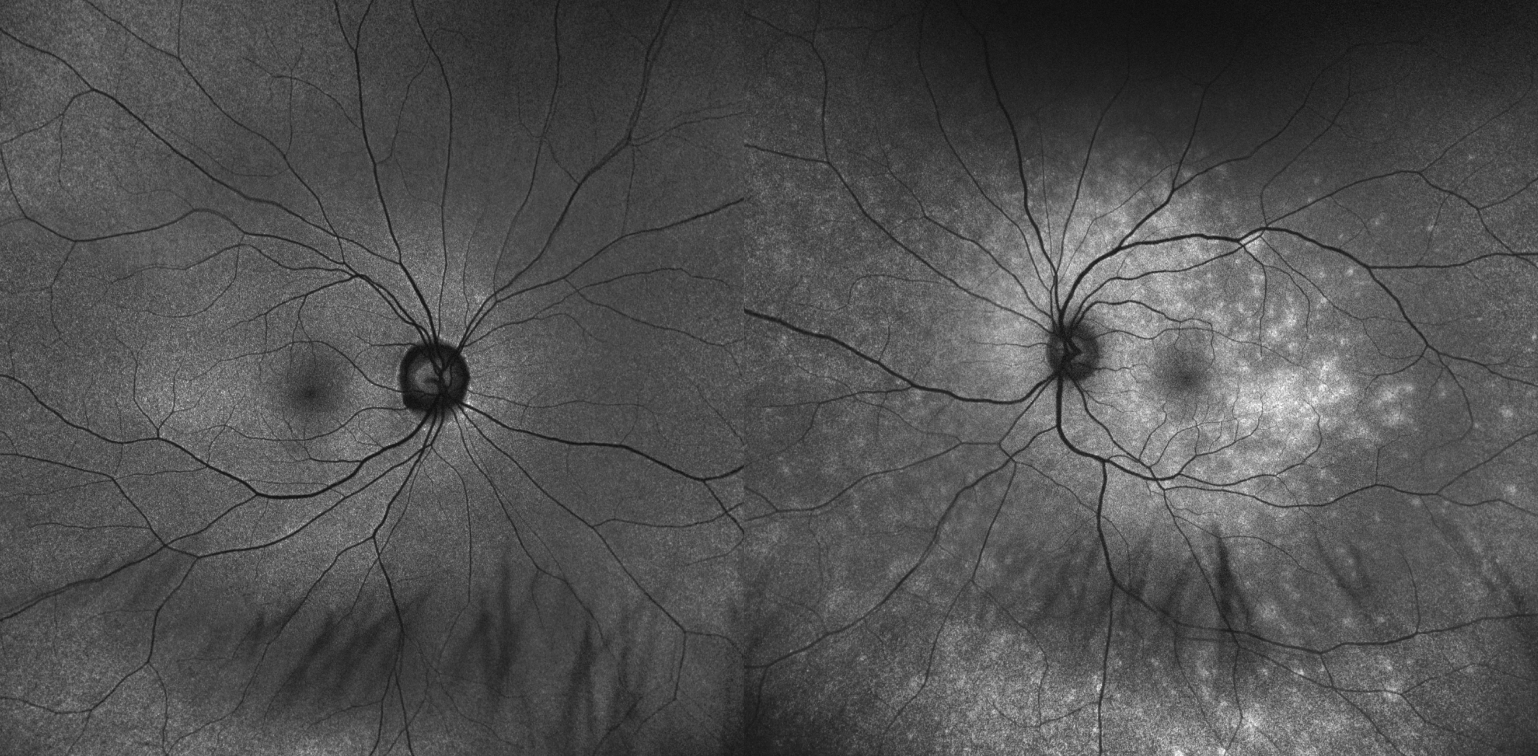 |
| Fig. 3. Montage FAF of the right and left eyes. Spotty hyperautofluorescence is seen throughout the posterior pole, coalescing in the macula of the left eye (right image). Click image to enlarge. |
Clinical findings in MEWDS include macular granularity and 100µm to 200µm transitory granular grayish spots through the posterior pole. Patients may also present with optic nerve edema and mild vitreous cell. Imaging modalities that can support a diagnosis include FAF, OCT and fluorescein angiography (FA). FAF classically demonstrates abnormal hyperautofluorescence with scattered lesions around the optic nerve and macula extending outwards. OCT imaging generally reveals outer retinal changes such as disruption of the retinal pigmented epithelium and ellipsoid zone that generally agree with the hyperautofluorescent areas on FAF. FA and indocyanine green angiography (ICG) may also used to evaluate MEWDS, and they reveal lesions that are hyperfluorescent on FA but hypocyanescent on ICG. The lesions on FAF and FA/ICG are often more apparent than those seen funduscopically.
Differentials
Other white dot syndromes are included in the differential diagnosis of MEWDS, and the presentation may have overlapping features with conditions such as multifocal choroiditis and panuveitis, acute zonular occult outer retinopathy, serpiginous choroidopathy, acute posterior multifocal placoid pigment epitheliopathy, birdshot chorioretinopathy and punctate inner choroidopathy. Additionally, autoimmune or infectious etiologies such as sarcoidosis, syphilis and tuberculosis should be considered. Interestingly, intraocular lymphoma has even been a documented masquerader.6 In the case of MEWDS, the diagnosis may be slightly more straightforward given that only a few of the aforementioned conditions also present unilaterally. The fundus lesions in MEWDS are also often finer and more fleeting than those seen in other differentials. The differentiation can often be made with a careful clinical examination, multimodal imaging and supporting laboratory studies.
Given the fact that the vast majority of patients have a full spontaneous recovery, MEWDS has been termed the “common cold” of the retina by one study.7 For this reason, intervention is typically not pursued. However, there are also reported cases in which the visual acuity did not recover completely. It has been suggested that the entering visual acuity is the strongest predictor of visual recovery, with a worse entering visual acuity portending a worse visual outcome.8,9
After ruling out other (particularly infectious) etiologies via bloodwork, some authors have used corticosteroids to hasten recovery. One such case describes the use of systemic corticosteroids for a young sumo wrestler who was anxious to improve his vision before an upcoming match.10 Though rare, patients can develop neovascular complications in MEWDS. Anti-VEGF agents have been used with success in many of these cases.11,12
Takeaway
Consider white dot syndromes in a patient who presents with blind spots, blurred vision and photopsias. In the case of a unilateral presentation and the previously described classic fundus findings, MEWDS should be at the top of our list. Remember other differential diagnoses, and pursue laboratory workup to rule out other etiologies. Although most patients experience a complete resolution of symptoms, careful monitoring can rule out progressive masquerading disease or an atypical course.
Dr. Bozung currently practices at Bascom Palmer where she primarily sees patients in the hospital's 24/7 ophthalmic emergency department. She also serves as the optometry residency program coordinator. Dr. Bozung is a fellow of the American Academy of Optometry and a member of the Florida and American Optometric Associations. She is a founding board member of Young OD Connect and serves on the editorial board for Review of Optometry. She has no financial interests to disclose.
|
1. Papasavvas I, Mantovani A, Tugal-Tutkun I, Herbort CP. Multiple evanescent white dot syndrome (MEWDS): update on practical appraisal, diagnosis and clinicopathology; a review and an alternative comprehensive perspective. J Ophthalmic Inflamm Infect. 2021;11(1):45. 2. Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for multiple evanescent white dot syndrome. Am J Ophthalmol. 2021;228:198-204. 3. Desarnaulds AB, Borruat FX, Herbort CP, Spertini F. Multiple evanescent white dot syndrome: a genetic predisposition? Klin Monbl Augenheilkd. 1996;208(5):301-2. 4. Yannuzzi NA, Swaminathan SS, Zheng F, et al. Swept-source oct angiography shows sparing of the choriocapillaris in multiple evanescent white dot syndrome. Ophthalmic Surg Lasers Imaging Retina. 2017;48(1):69-74. 5. Kang HG, Kim TY, Kim M, et al. Expanding the clinical spectrum of multiple evanescent white dot syndrome with overlapping multifocal choroiditis. Ocul Immunol Inflamm. 2022;30(1):81-9. 6. Russell JF, Pichi F, Scott NL, et al. Masqueraders of multiple evanescent white dot syndrome (MEWDS). Int Ophthalmol. 2020;40(3):627-38. 7. Tavallali A, Yannuzzi LA. MEWDS, common cold of the retina. J Ophthalmic Vis Res. 2017;12(2):132-4. 8. Barile GR, Harmon SA. Multiple evanescent white dot syndrome with central visual loss. Retin Cases Brief Rep. 2017;11 Suppl 1:S219-25. 9. Takahashi Y, Ataka S, Wada S, Kohno T, Nomura Y, Shiraki K. A case of multiple evanescent white dot syndrome treated by steroid pulse therapy. Osaka City Med J. 2006;52(2):83-6. 10. Bosello F, Westcott M, Casalino G, et al. Multiple evanescent white dot syndrome: clinical course and factors influencing visual acuity recovery. Br J Ophthalmol. 2022;106(1):121-7. 11. Wyhinny GJ, Jackson JL, Jampol LM, Caro NC. Subretinal neovascularization following multiple evanescent white-dot syndrome. Arch Ophthalmol. 1990;108(10):1384-5. 12. Battaglia Parodi M, Iacono P, Zucchiatti I, Bandello F. Choroidal neovascularization associated with multiple evanescent white dot syndrome treated with intravitreal ranibizumab. Ocul Immunol Inflamm. 2018;26(4):608-11. |

