 |
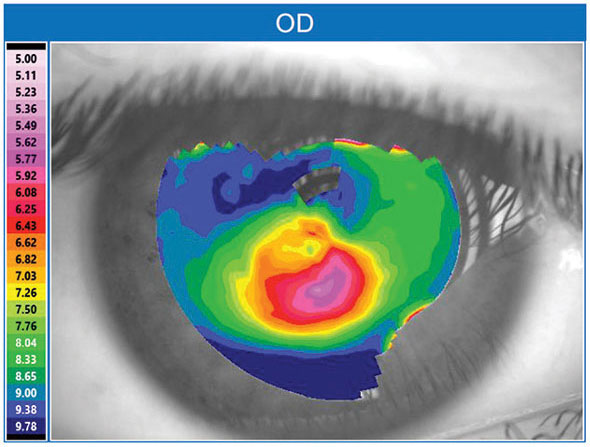
| Heating the cornea to induce collagen shrinkage—thermokeratoplasty—seems to work well for KCN patients. Photo: Brian Chou, OD |
Though it never really took off as a mainstream treatment, thermokeratoplasty (TKP) has been used in the past as an alternative to penetrating keratoplasty for cases of advanced keratoconus. The thermokeratophore used in the treatment offers controlled shrinkage of corneal collagen that alters the corneal curvature in these patients. Many different surgical methods for TKP have been reported in the literature, leading to variation in surgical outcome. While not routinely used today, TKP was nevertheless recently reported to produce good long-term outcomes. The 30-year follow-up study is the longest report on TKP outcomes to date.
The retrospective study (April 1979 to December 1991) reviewed 2,949 patients with keratoconus in the Kyoto Prefectural University of Medicine’s clinical database and included 42 patients (29 male, 13 female) who had more than 30 years of postoperative follow-up. These patients first presented at an average age of 23.4 and underwent unilateral TKP. Mean follow-up was 35.2 years, and no adverse events or complications, such as infectious keratitis, corneal perforation, corneal melting and/or bullous keratopathy, were observed.
Eleven of the 42 eyes underwent corneal transplantation at an average of 24.9 years postoperatively due to an inability to wear contact lenses continuously and were able to resume continuous wear post-transplant. The authors observed good outcomes over the long-term postoperative period.
The researchers speculate that variations in the TKP probe temperature may account for some of the variable outcomes in the other studies. While their team did not detect any cases of corneal melting or perforation, previous studies have reported delayed epithelial healing and stromal melting postoperatively. The Kyoto group set the TKP probe to between 80° and 90° Celsius, which is lower compared with other reports that used temperature settings of 90° to 95° and as high as 110° in some cases. “Although other factors related to the amount of heat given to the cornea, such as corneal thickness and probe contact time, need to be verified, in addition to histological findings, it’s possible that the temperature of the probe affected the results,” the researchers wrote.
They were pleased by the number of patients able to continue or resume contact lens wear after TKP. “By flattening the cornea and reducing the size of protrusion, TKP is expected to not only reduce corneal astigmatism but also facilitate contact lens wear,” they explained. “In our results, 31 of 42 eyes were able to continue wearing contact lenses without corneal transplantation. Even in the 11 eyes that underwent corneal transplantation, it was estimated that continuous contact lens wear was possible until corneal transplantation was performed.”
Itoi M, Higashihara H, Yamagishi K, et al. Thermokeratoplasty for keratoconus: a more than 30-year follow-up study. Cornea. 2021;00:1-4. |


