 |
|
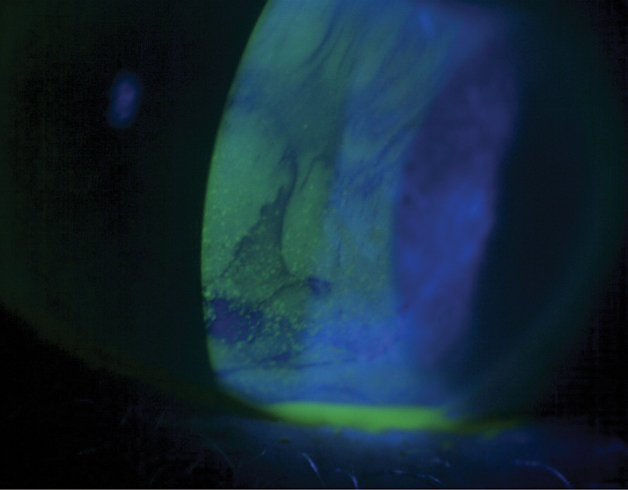
Tear meniscus is an important indicator of sufficient tear volume, and optimal tear quality is needed for a healthy tear film turnover. Photo: Jack Schaeffer, OD. Click image to enlarge. |
Increased risk of dry eye is associated with the use of contact lenses (CLs) and tear volume decreases gradually over time with CL wear. Consequently, researchers from Turkey wanted to study if tear meniscus parameters in CL wearers may indicate dry eye.
To study this question, they prospectively included 50 soft lens wearers and 25 healthy non-CL wearers as controls. Subjects were categorized into three groups of 25 each: symptomatic CL wearers, asymptomatic CL wearers and non-CL wearers. Soft lenses were fitted on each eye of wearers and lower tear meniscus was imaged with OCT before and immediately after insertion, then reimaged at two, five and 10 hours after insertion.
The researchers found that at baseline, tear film turbidity and a metric they called “percentage area occupied by particles” (PAOP) measurements were higher in the symptomatic group than the others. In all groups, there was no difference between tear meniscus height, tear meniscus depth, turbidity and PAOP at baseline visit and two hours after insertion. However, the symptomatic CL group displayed significant decrease in tear meniscus height and depth in the fifth hour. As well, turbidity and PAOP measurements were significantly higher in both symptomatic and asymptomatic wearers than non-wearers at five and 10 hours. It should also be noted that tear meniscus height and depth decreased throughout the day in all participants.
In the discussion section of their paper, published recently in Graefe’s Archive for Clinical and Experimental Ophthalmology, the authors expand upon their findings, recording that symptomatic wearers had significantly lower baseline tear break-up time and Schirmer I scores as well as higher Ocular Surface Disease Index scores than the other groups. This group’s baseline turbidity and PAOP results were lower, though, which could be due to incidence of meibomian gland dysfunction or increase in inflammatory cells and tear meniscus osmolarity which increase in CL wearers, especially in symptomatic ones.
In the last OCT examination at 10 hours of wear, the all-tear meniscus parameters were significantly changed compared to baseline in CL wearers; turbidity and PAOP values in both symptomatic and asymptomatic groups were higher than those in the non-CL group at 10 hours. As the study authors explain, reduced tear meniscus volumes and increased tear osmolarity may be caused by a diminished mucin and lipid layer on the lens surface with a long time of CL wear and increased tear evaporation. It is further hypothesized that increased inflammatory cells, decreased tear meniscus volume and tear hyperosmolarity would lead to higher tear meniscus turbidity and PAOP values in both symptomatic and asymptomatic wearers. Succinctly, the authors put it that “as the number of hours spent wearing contact lenses increases throughout the day, this can lead to an increase in the factors that play a role in the increase of tear film turbidity and PAOP.”
They add that these results may be helpful clinically, as “turbidity and PAOP may be measures of how well the tear film and meniscus are functioning and they may be one of the indicators of dry eye in soft CL wearers. Lastly, spectral-domain OCT can be helpful in the non-invasive evaluation of tear meniscus in CL wearers.”
Dogan L, Arslan GD. The analysis of tear meniscus parameters during daily soft contact lens wear using optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. August 7, 2024. [Epub ahead of print]. |


