 |
|
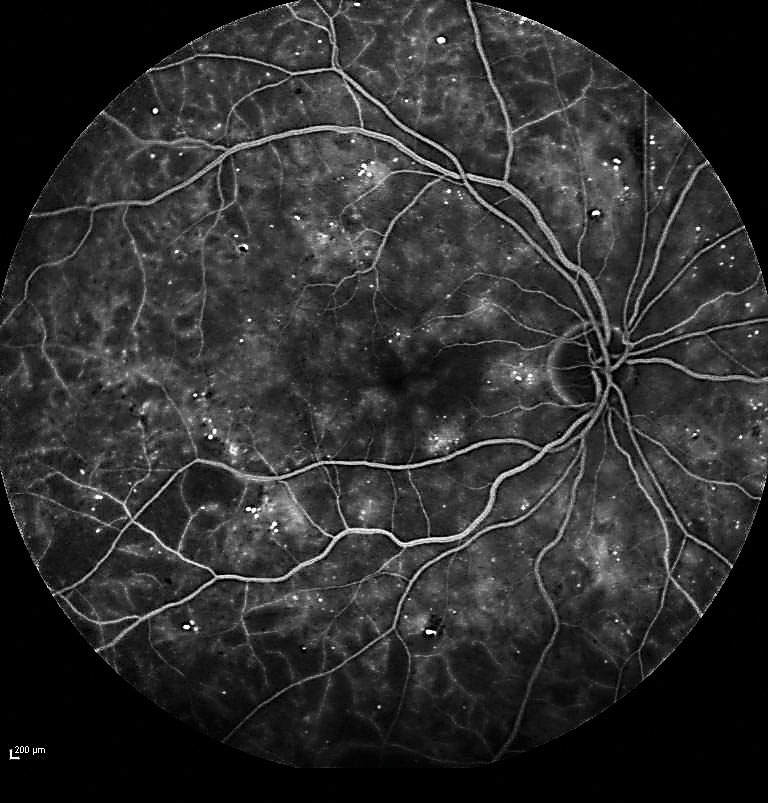
A new study in AJO highlights how different diabetes subtypes lead to varying rates of retinal thinning. Researchers found that patients with severe insulin-deficient and severe autoimmune diabetes experienced the fastest choroidal thinning, while those with severe insulin-resistant diabetes had the most significant loss of ganglion cell layers. These findings suggest that personalized screening intervals might be crucial for early detection and management of diabetic retinopathy in at-risk populations. Photo: Jay M. Haynie, OD. Click image to enlarge. |
As individuals with diabetes age, they’re at greater risk for thinning of the choroid and ganglion cell-inner plexiform layer (GC-IPL). Studies have shown that each subtype of the disease progresses differently, and some are more closely associated with certain vascular and neurological risks than others. A new study in American Journal of Ophthalmology followed patients over a four-year period to watch how various subtypes of diabetes mellitus (DM) impact the rates of choroidal GC-IPL thinning. Using swept-source OCT, they observed significant microvascular damage in some patients and early signs of neurodegeneration in others, suggesting that shortening screening intervals may be warranted.
Type 2 DM patients in this prospective, observational, longitudinal study, conducted in China, were categorized into five groups: severe autoimmune DM, severe insulin-deficient DM, severe insulin-resistant DM, mild obesity-related DM and mild age-related DM. OCT was used to measure baseline and four-year follow-up thicknesses of the relevant structures. A total of 1,070 patients (59.1% female) were included for cluster analysis, with an average age of 64.3.
Over a median 4.1-year follow-up, both choroidal and GC-IPL thickness decreased significantly across all groups. Choroidal thinning was most pronounced in the insulin-deficient (-6.5μm/year and -3.5%/year) and autoimmune (-6.27μm/year and -3.19%/year) groups, while thinning was the slowest in those with age-related diabetes (-3.63μm/year and -1.98%/year). The greatest GC-IPLT loss was exhibited in the insulin-resistant group (-0.66μm/year and -0.91%/year), and the least in insulin-deficient subjects (-0.36μm/year and -0.49%/year).
The study authors noted in their paper that these findings suggest that such losses may precede clinical manifestations of diabetic retinopathy (DR) in type 2 diabetes patients and highlight the course of microvascular damage and early neuronal loss in those with insulin-deficient and insulin-resistant diabetes, respectively.
Notably, subjects with insulin deficiency exhibited the most pronounced vascular damage among all diabetes subtypes, with an accelerated choroidal thinning rate of -2.89μm/year compared to those with mild age-related diabetes, they continued. “This underscores that DM patients with immune deficiencies or severe insulin deficiencies may experience accelerated [choroidal] thinning compared to older DM populations,” they wrote. Furthermore, the study highlights early signs of neuronal damage in the insulin-resistant DM group. “Our findings reveal an overall GC-IPLT thinning rate of -0.49μm/year in DM patients, with significant variation among DM subtypes.”
The observed thinning occurred in both patients with and without DR, noted the authors, which they say suggests these changes could be potential indicators of early microvascular and neurophysiological alterations preceding clinical DR onset. Among DM patients without diabetic retinopathy, the researchers observed significant differences in choroidal thinning rates between the insulin-dependent and age-related groups, as well as in GC-IPLT thinning rates between the insulin-resistant and age-related subtypes. “These distinctions in non-DR patients may indicate processes of choroidal vascular decline and retinal neurodegeneration, highlighting diverse neurovascular mechanisms across different metabolic states of DM during early DR stages.”
Due to the challenges in non-invasively detecting early retinal neurodegeneration or choroidal changes in early DM stages, the results of this study demonstrate the potential for shortened screening intervals in high-risk populations, notably insulin-dependent DM patients with accelerated choroidal thinning and insulin-resistant patients with accelerated GC-IPLT thinning. “For DR patients requiring treatment, changes in CT and GC-IPLT could serve as biomarkers for assessing treatment efficacy, guiding adjustments in therapies targeting vascular endothelial growth factor and neurotrophic factors.”
The strengths of this study lie in its prospective longitudinal design with extended follow-up, as well as its high-quality OCT imaging, the authors noted in their paper. However, they acknowledged that limitations include the lack of ethnic diversity, failure to account for the influence of diurnal fluctuations in OCT-measured values and the omission of functional ocular changes as a metric considered.
Ultimately, as this study identified accelerated thinning before clinical manifestations of DR, particular attention may be warranted in specific groups to potentially improve prognostication and reduce rates of blindness, the authors concluded.
Liu K, Li T, Zhong P, Zhu Z, et al. Longitudinal changes in retina and choroid across novel subtypes of diabetes mellitus. American Journal of Ophthalmology. September 3, 2024. [Epub ahead of print.] |


