 |
|
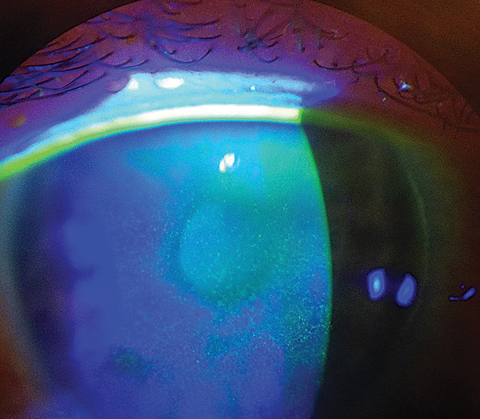
A phase IV postmarket study of three artificial tears found, as one would expect, positive outcomes from the regimen on dry eye patients. Likely more interesting was the influence of differing urban environmental conditions on dry eye signs and symptoms. Photo: Scott G. Hauswirth, OD. Click image to enlarge. |
The Tear Film and Ocular Surface Society’s (TFOS) Dry Eye Workshop II (DEWS II) made great strides in linking symptoms of dry eye disease (DED) with behavioral and environmental factors. In particular, it shed light on the impact of air pollution and temperature on those with signs of dry eye. To test the influence of these variables on DED symptoms, researchers in Mexico conducted a clinical trial by putting participants on a regimen of ocular lubricants. After one month, individuals lowered their Ocular Surface Disease Index (OSDI) score and increased their tear breakup time.
Published in Clinical Ophthalmology, this was a Phase IV randomized open-label clinical trial conducted at six metropolitan sites in Mexico. Of the 173 participants diagnosed with mild-to-moderate DED, 161 completed the entire protocol. Mean age was 30.7 (range 18 to 71 years) and 56.6% of subjects were female. Individuals were randomly assigned to receive one of three different preservative-free artificial tears QID for 30 days in both eyes.
The results of the study show, after using sodium hyaluronate–based ocular lubricants for a month, patients had significant improvement in ocular comfort. OSDI score decreased by 14.8 points, fluorescein staining score decreased by 0.3 points, and non-invasive tear film break-up time (NIBUT) increased by 2.9 seconds. “The improvement was directly linked to the duration of eye drop usage,” the authors wrote in the study. “Additionally, the results show that patients living in cities with cooler weather, high humidity and low air quality […] have OSDI scores up to 4.4 points higher than those who live in cities with similar pollution and humidity levels, but with higher temperatures.”
When exploring the association of increased ground-level ozone, NO2, and PM2.5 concentrations and increased ocular discomfort and irritation, the authors say their research didn’t indicate a direct impact of any air particle on fluorescein or lissamine green staining scores; however, they did observe an increase in fluorescein score by 0.03 for each grade of rising maximum temperature levels during hot seasons. “The present study shows that for patients recruited in summer and autumn, we can expect longer NIBUT values compared to those recruited in spring, up to 2.9 seconds,” they wrote, likely influenced by lower ozone levels in winter.
Although there was no evidence to suggest one ocular lubricant was more effective than its counterpart, the researchers said the severity of the symptoms of DED decreased significantly over time with the use of the sodium hyaluronate–based ocular lubricants.
A limitation of this study is the subjective experience of DED symptoms, as evaluated by the OSDI questionnaire. The authors cite its limited account of the effects of DED on vision-related functioning as opposed to severity alone. They also noted the lack of details about the specific working conditions of their patient population, including commute time and screen time as potential study limitations. “Lastly, the absence of a control group or placebo would limit the observed changes in the OSDI and signs over the month of treatment,” they wrote.
In conclusion, the study draws a correlation between environmental factors on the clinical signs and symptoms of mild-to-moderate DED. “Patients who live in densely populated cities with high heavy traffic, and poorly controlled air pollution can benefit from using ocular lubricants to improve their symptoms,” wrote the authors.
Muñoz-Villegas P, García-Sánchez G, Jauregui-Franco RO, Quirarte-Justo S, Sánchez-Ríos A, Olvera-Montaño O. Influence of environmental factors with clinical signs and symptoms in the management of dry eye disease. Clinical Ophthalmology. August 30, 2024. [Epub ahead of print.] |


