 |
|
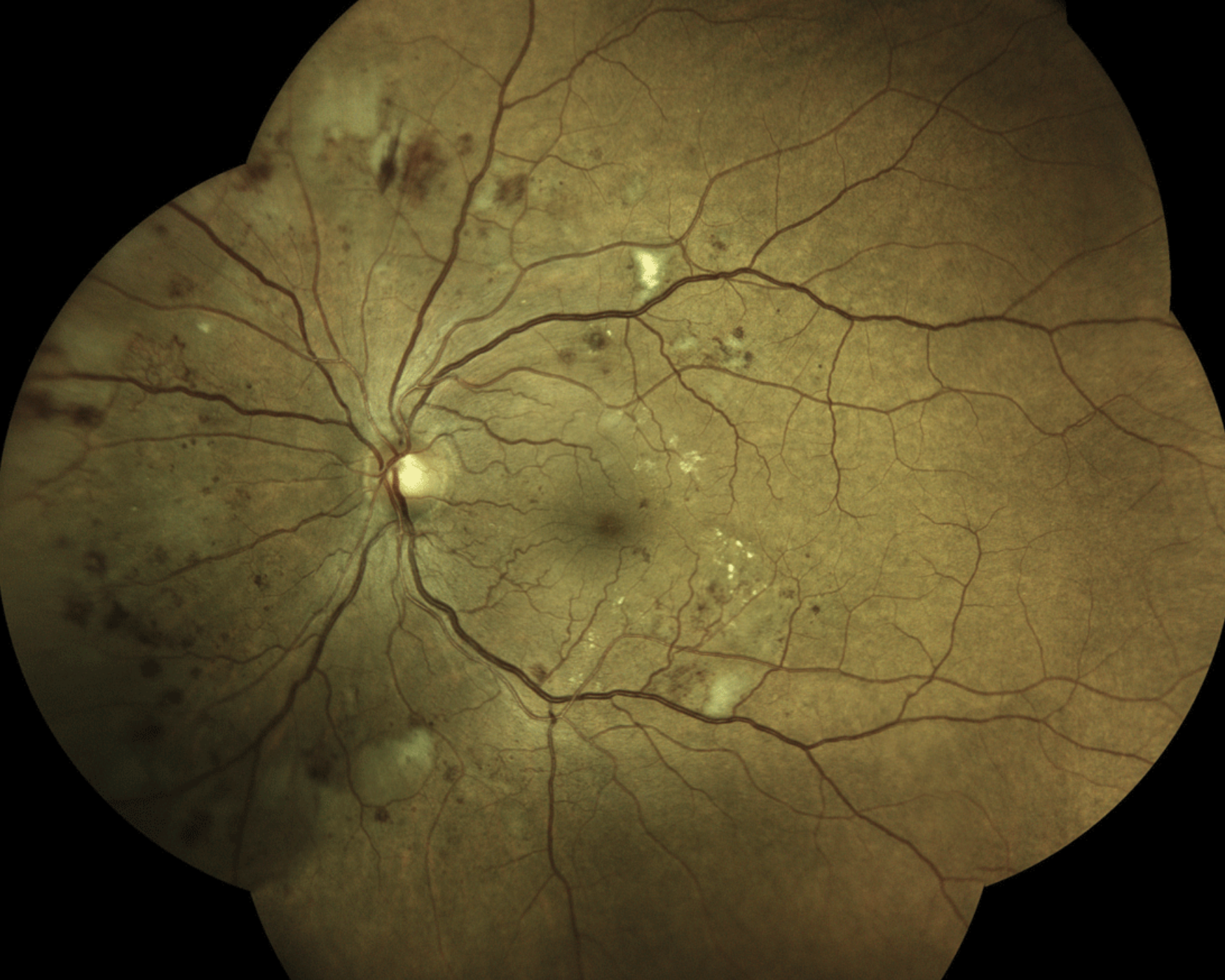
While using PRP and anti-VEGF injections in the initial treatment of proliferative diabetic retinopathy is an approach gaining popularity among clinicians, the optimal order of these interventions remains to be investigated. Photo: Steven Ferrucci, OD. Click image to enlarge. |
Initial treatment of patients with proliferative diabetic retinopathy often involves a combined approach using panretinal photocoagulation (PRP) and anti-VEGF injections. Large randomized clinical trials usually prefer monotherapy, limiting the information available on the outcomes of combined treatment approaches and whether the sequence of PRP and anti-VEGF therapy has an effect. A new study published in JAMA Ophthalmology aimed to close this research gap by comparing the need for pars plana vitrectomy (PPV) among patients treated with PRP first then anti-VEGF injections and vice versa.
The retrospective cohort study included more than 3,000 patients with new PDR diagnoses from the TriNetX EHR network, stratified by therapy with PRP and subsequent anti-VEGF or anti-VEGF and subsequent PRP. While the primary outcome was the need for PPV, secondary outcomes included incidence of PPV, vitreous hemorrhage or tractional retinal detachment. After propensity score matching, which controlled for baseline demographic characteristics and medical comorbidities, there were 1,377 patients in each of the two treatment groups. The average age was 63 years in both groups, and the sex ratio was nearly 50:50.
The results showed that patients in the PRP-first group demonstrated a higher risk of needing PPV over the course of five years compared to those in the anti-VEGF-first group, with similar associations at six months, one year and three years. This group also had higher rates of vitreous hemorrhage and tractional retinal detachment at the same four time points.
“While combined therapy for the treatment of PDR has gained popularity in clinical practice, as shown by the ASRS PAT surveys, if this study’s approach is considered, it is unknown if the order of treatment modalities affects outcomes,” the researchers explained in their JAMA Ophthalmology paper. They cited one previous study that found “PRP after intravitreal conbercept injections (Lumitin; Kanghong Biotechnology) was associated with a reduced number of subsequent anti-VEGF injections compared with eyes treated with PRP before intravitreal conbercept at two years [six vs. 8.5 injections], despite no difference in visual and anatomic outcomes between cohorts.”
Furthermore, in the present study, which used a large, heterogenous, real-world database of matched patients with PDR, “administration of PRP first was associated with an increased risk of undergoing PPV, as well as developing vitreous hemorrhage and tractional retinal detachment, compared with anti-VEGF injection [first],” the study authors wrote.
While the literature on this topic is growing, they caution that further research is still warranted to determine the optimal order of PRP and anti-VEGF injections for treating PDR, especially considering the increasing popularity of this combined approach.
Alsoudi AF, Wai KM, Koo E, et al. Initial therapy of panretinal photocoagulation vs anti-VEGF injection for proliferative diabetic retinopathy. JAMA Ophthalmol. August 29, 2024. [Epub ahead of print]. |


