 |
|
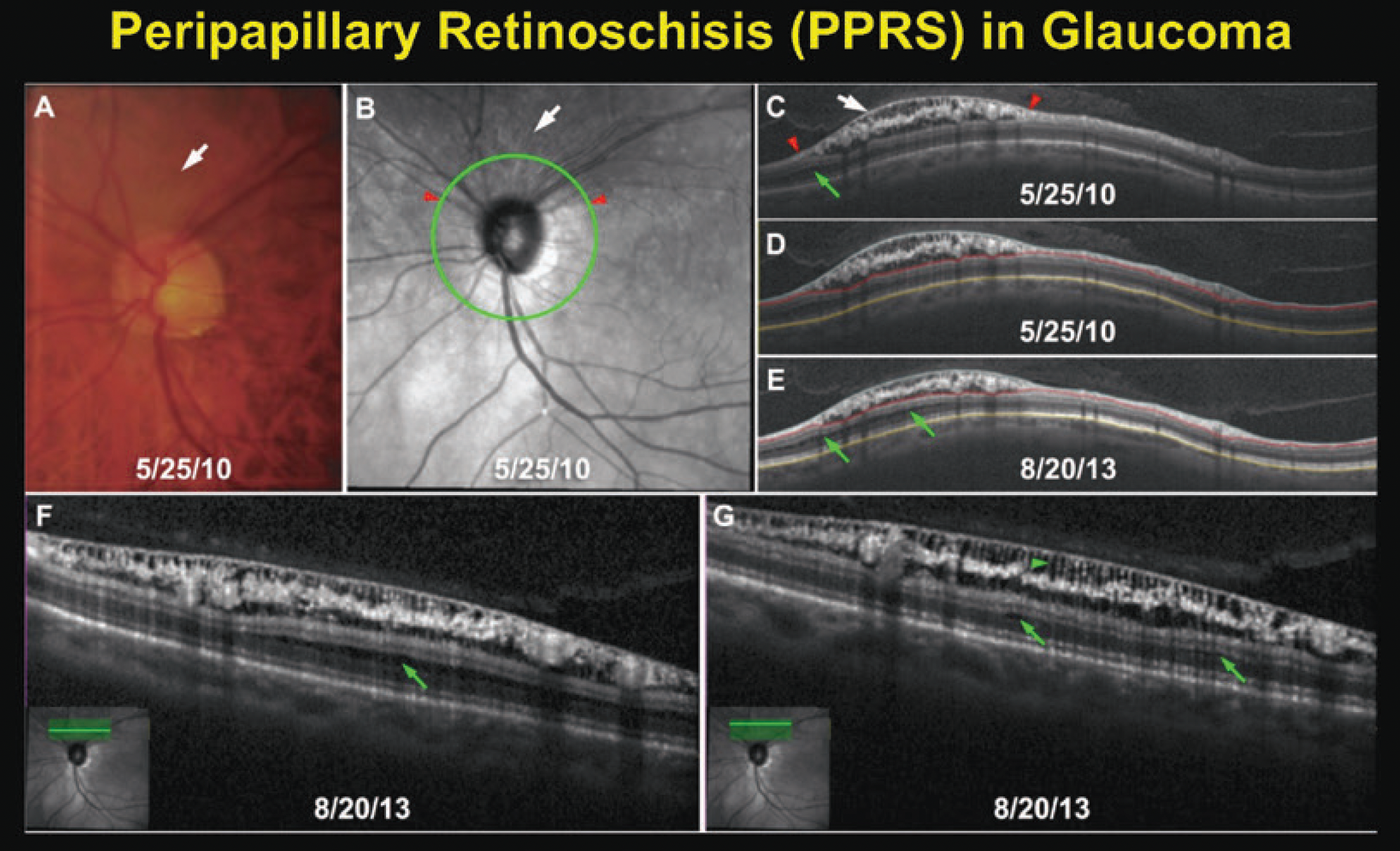
Optometrists should exercise caution when interpreting OCT data for glaucoma patients in the presence of peripapillary retinoschisis, study warns. Photo: Brad Fortune, OD, PhD. Click image to enlarge. |
The increased use of OCT has revealed that peripheral paracentral retinal splitting (PPRS) is more common in glaucoma patients than previously recognized. This finding could have potential implications for the accuracy of measurements such as RNFL thickness and the monitoring of disease progression. A recent study that aimed to shed light on the relationship between PPRS and glaucoma identified several correlations between PPRS and RNFL and visual field changes.
The researchers performed a systematic review of 10 relevant studies published in four leading online databases. Of these, seven were case-control, one was a cohort study and two were case series.
Six of the 10 studies showed that peripapillary retinoschisis often overlapped pre-existing RNFL defects. In one, the de novo development of peripapillary retinoschisis was reported to be more frequent in eyes with glaucoma progression than in eyes without progression. Visual field findings were inconsistent among the studies, with just one of six showing that glaucoma patients with peripapillary retinoschisis had faster visual field deterioration than those without it. As for the connection between peripapillary retinoschisis and glaucoma progression, two out of seven studies associated the finding with faster progression.
Regarding RNFL thickness, the researchers pointed out in their paper for Journal of Glaucoma that “several authors noted thicker RNFL in PPRS eyes, followed by an important decrease in RNFL thickness after resolution of PPRS, potentially complicating glaucoma monitoring with OCT” and making it difficult to assess the degree of damage. While studies had conflicting findings, the researchers found that in general, “it was observed that the rate of RNFL thinning could be faster in glaucomatous eyes with PPRS than controls (eyes with glaucoma without PPRS).”
| For more on PPAS, see the article by Brad Fortune, OD, PhD in this recent publication by the Optometric Glaucoma Society. |
While the RNFL was the most frequently involved layer in PPRS in six out of seven studies, the researchers recognized in their paper that “retinoschisis is not confined to the RNFL nor solely located in the peripapillary area.” While not covered in this review, the association between macular retinoschisis and glaucoma, for example, may be valuable to investigate in the future.
Likewise, the authors noted that it’s relevant “to recognize that schisis is not exclusive to the retina; schisis has been observed in the prelaminar tissue, particularly in individuals with glaucoma.” They explained, “Prelaminar tissue schisis could reflect ongoing structural alterations resulting from glaucomatous deformation and remodelling of the optic nerve head, potentially attributed to mechanical breakdown of the load-bearing connective tissues.” Prelaminar tissue schisis may also serve as a risk factor for subsequent damage, they added.
In summarizing their findings, the study authors highlight that “PPRS serves as a confounding factor in the OCT structural analysis of glaucoma. This underscores the need for caution when interpreting serial RNFL data, so as not to overestimate RNFL thickness when PPRS is present or misinterpret the resolution of retinoschisis as rapid structural progression,” they concluded.
Almeida MC, Ribeiro M, Barbosa-Breda J. Peripapillary retinoschisis in glaucoma: a systematic review. J Glaucoma. May 2024. [Epub ahead of print]. |


