 |
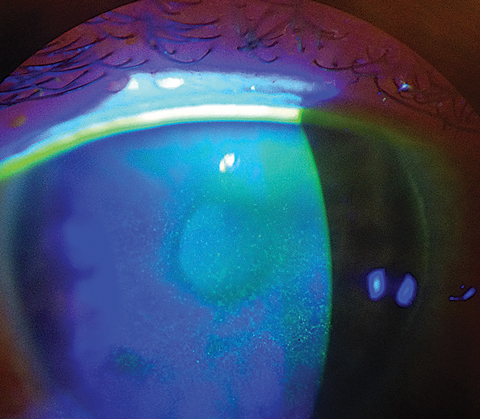
| Researchers hope the results of their survey will prompt clinicians to update their dry eye care and patient education methods to better meet the needs of patients. Photo: Scott G. Hauswirth, OD. Click image to enlarge. |
It’s well-known that the prevalence of dry eye disease (DED) is increasing and the condition can decrease patients’ quality of life. In a newly published paper, researchers report on a survey-based study performed to take a deep dive into aspects of care not normally explored during patients’ office visits, such as the time required for disease care, financial cost of treatment and patients’ preferred sources of information. Several findings were somewhat surprising. They found that almost one-fourth of patients spend an hour or more on daily treatment regimens, meibomian gland expression was uncommon, ophthalmologists provided two-thirds of all dry eye care and half of respondents reported that their eyecare provider is not their primary source of information.
An electronic survey was emailed to online dry eye newsletters and support groups. In total, 639 people with self-reported dry eye responded (86% women, 14% men). Artificial tears were the most reported intervention (76% initially after diagnosis, 71% currently), which was not a surprise to the authors and validates that they provide some level of dry eye relief without adding an unreasonable burden of care.
Treatments aimed at addressing evaporative dry eye were underused, such as proper eyelid hygiene (less than 25%) and in-office meibomian gland expression (less than 4%). Initial and current use of warm compresses was reported by less than 50%. Respondents were more likely to report that eyelid hygiene was part of their current treatments than their initial therapy.
“Warm compresses and eyelid hygiene require more time than instilling an eye drop, and results are not as immediately rewarding; therefore, therapy that focuses on managing eyelid contributions to DED may seem overly burdensome to some patients,” the researchers explained in their paper on the survey for Eye & Contact Lens. “Whether these treatments were recommended but not adopted by our survey respondents was not queried, but of importance, the patients reported that they did not use basic, common sense therapies that are known to improve symptoms.” The researchers notes that barriers to undergoing in-office meibomian gland therapies “may include equipment cost, the substantial operational infrastructures required to provide such services and lack of insurance coverage.”
The survey asked about both initial and current prescription therapies used by dry eye patients. However, it’s worth noting that this survey was conducted in 2018 and thus does not reflect current prescribing patterns, as several recently approved dry eye drugs were not available at the time. Restasis (Allergan) was the only approved cyclosporine drug when the survey was conducted and Xiidra (Bausch + Lomb) was less than two years into its commercial availability. Cequa (Sun Pharma), Vevye (Harrow Health), Eysuvis (Alcon), Tyrvaya (Oyster Point) and Meibo (B+L) had not yet been approved.
From a 2018 vantage point, however, approximately 25% of those surveyed reported initial treatment with Restasis, and 20% reported current (as of the time of survey) use of this medication. Participants categorized to be in the long-term phase of care (six to 10 years) reported the highest initial use of Restasis (31%), yet only 20% of that same group reported continued use. Among recently diagnosed patients, 24% reported initial use and 22% reported current (2018) use of 0.05% cyclosporine. Lifitegrast, launched in 2016, was used by 7% of respondents in the 2018 survey, the authors added.
What authors found noteworthy was that most respondents used three therapeutic options on average regardless of time since their diagnosis. “The consistent use of multiple therapeutic options suggests that monotherapy may not provide adequate symptomatic relief, even in newly diagnosed DED,” the authors explained. “When the burden of care, costs of multimodal therapy or both become unacceptable, patient compliance tends to wane.”
Management of DED is clearly a time burden for patients, the study shows. “Although more than half of respondents reported spending 20 minutes or less a day for dry eye self-management, 22% reported that their therapy required an hour or more daily. Not only is an hour a considerable amount of time, but this time is frequently distributed throughout the day, requiring patients to disrupt their activities to deal with their chronic disease,” the authors wrote. “This may result in reduced work productivity and quality of life. Eye care clinicians should thoughtfully prescribe therapeutic regimens that will address the primary cause and secondary effects of disease while minimizing the burden of interventions.”
In addition, 55% estimated devoting five to 20 minutes daily on self-management; 22% spent an hour or more. Ophthalmologists provided most dry eye care (68%) to the surveyed population (vs. 26% by optometrists). Only 48% reported that their primary source of dry eye information came from their eye care clinician, which was concerning to the authors. Instead, nearly half of respondents used online resources (internet searches, 29%; online support groups, 19%) as their primary sources of current information about their condition.
“Although reputable sources of information exist (e.g., foundations dedicated to a particular disease, selected DED–focused websites), misinformation that may directly contradict evidence-based recommendations may also be encountered in this unregulated environment,” the authors noted. “Eyecare clinicians would be well advised to ensure that their patients with dry eye thoroughly understand the pathophysiologic characteristics of their disease and all appropriate treatment options.”
Lastly, and one of the most important findings of the study, the authors found that managing dry eye creates an economic burden for patients. “The estimated mean annual cost of disease management was $1,578 for all respondents regardless of disease duration,” the authors explained. When only US participants were analyzed, the average yearly out-of-pocket cost of dry eye treatment was $1,294—a 65% increase from 2008. This increase could reflect the availability of new therapies not covered by insurance. As out-of-pocket costs increase, patients on fixed incomes and those with limited insurance coverage may forego recommended treatments, the authors concluded.
"This study provided a unique opportunity to hear directly from patients on how their eye condition impacts their daily life and finances,” says Ellen Shorter, OD, of the University of Illinois, one of the researchers. “Most of the individuals in this study received care from an ophthalmologist (68%) rather than an optometrist (26%). Interestingly, less than half of the participants indicated their primary spruce of information of DED was obtained from their eye care provider with many obtaining information from the internet and online support groups. Clinicians should take the opportunity to educate their patients about dry eye management and provide resources."
Nau CB, Nau AC, Fogt JS, et al. Patient-reported dry eye treatment and burden of care. Eye & Contact Lens. February 19, 2024. [Epub ahead of print.] |


