 |
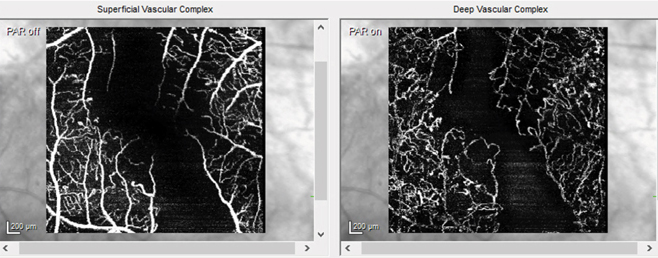
An early warning sign of cognitive issues may be seen in loss of retinal microvascular perfusion on OCT-A (shown here in an unrelated diabetic retinopathy patient). Photo: Jessica Haynes, OD. Click image to enlarge. |
Research shows a staggering 50% of patients with amnestic mild cognitive impairment (MCI) will eventually progress to Alzheimer’s disease. It’s not a complete surprise, given that these individuals share many clinical features with Alzheimer’s disease patients and have a higher yearly risk of disease progression and non-amnestic MCI than the general population. In a recent study, researchers assessed retinal microvascular alterations in those with and without MCI using OCT angiography (OCT-A).
A total of 112 eyes of 59 amnestic MCI participants, 32 eyes of 17 non-amnestic MCI participants and 111 eyes of 56 controls with normal cognition were included. In addition to OCT-A, vessel density and perfusion density in the Early Treatment Diabetic Retinopathy Study (ETDRS) 3mm circle and ring were assessed. Retinal thickness parameters including retinal nerve fiber layer (RNFL) thickness, ganglion cell-inner plexiform layer thickness, central subfield thickness and choroidal parameters such as subfoveal choroidal thickness were also analyzed.
OCT-A showed that individuals with amnestic MCI have decreased retinal perfusion density compared with controls and non-amnestic MCI participants. However, the authors did not observe significant differences in retinal or choroidal thickness parameters among or between groups after adjusting for age and sex, which aligns with findings from a previous study.
“With regard to RNFL thickness, early gliosis may serve as a potential explanation for the equivocal results of both studies,” the authors explained. “While retinal thinning may occur in the late stages of Alzheimer’s disease, early gliosis may occur in the setting of active neurodegeneration. As a result of such gliosis, OCT analysis may be unable to detect any significant difference in RNFL thickness earlier in the clinical spectrum of Alzheimer’s disease.”
They noted that as the disease progresses, retinal thinning may begin to outpace gliosis, ultimately allowing for detection with OCT.
Significant differences in perfusion density were found between both amnestic and non-amnestic MCI patients compared with controls with normal cognition within the 3mmx3mm ETDRS ring. The authors suggested 3mmx3mm OCT-A is the preferred method for detecting novel biomarkers in amnestic and non-amnestic MCI patients because these scans may be more useful in identifying subtle macular microvascular changes.
“These results highlight the potential use of retinal microvascular density measures as potential noninvasive biomarkers to help distinguish amnestic MCI within the broad category of cognitive impairment,” the authors concluded. “Earlier identification of this clinically relevant subcategory of patients may be important, as this group serves as a high-risk population for eventual progression to Alzheimer’s disease and may potentially benefit from disease-modifying therapies.”
Robbins CB, Akrobetu D, Ma JP. Assessment of retinal microvascular alterations in individuals with amnestic and non-amnestic mild cognitive impairment using optical coherence tomography angiography. Retina. February 17, 2022. [Epub ahead of print]. |


