Prior studies suggest that diabetes and age may play a role in the development of corneal decompensation following cataract surgery, but most have been done in primarily small sample sizes. In a large new study, researchers sought to identify the demographic and systemic risk factors associated with the development of corneal edema and the need for corneal transplantation following cataract surgery using a large nationwide dataset of Medicare beneficiaries and found Asian, Hispanic and North American Native race is the highest factor, followed by age and diabetes.
 |
|
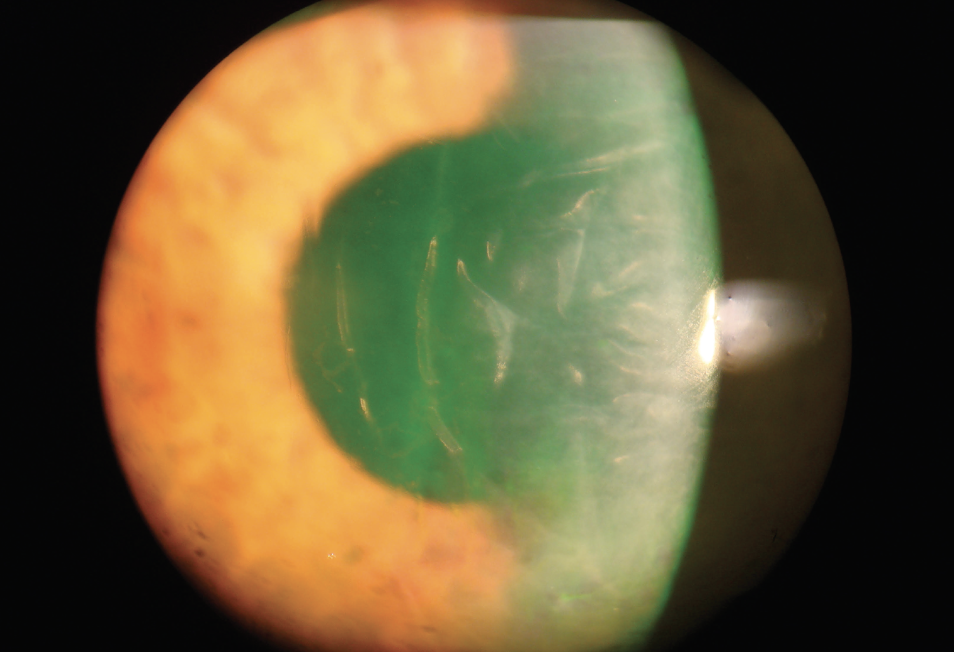
Racial and ethnic minorities were found to be the highest risk of corneal edema, but further research is needed to understand these underlying factors. Photo: Derek Cunningham, OD. Click image to enlarge. |
A total of 187,746 Medicare beneficiaries aged over 65 years who received cataract surgery with at least one year of continuous follow-up were included. Of those, 67,734 had diabetes. The main outcome was the association between demographic characteristics such as age, sex and race/ethnicity, and systemic factors including diabetes status, hypertension and tobacco use on the incidence of corneal edema and the subsequent need for corneal transplantation following cataract surgery.
Increasing age and race were found to be significant risk factors for developing corneal edema after controlling for sex, tobacco use and systemic factors. Compared to those between the ages of 65 and 74, beneficiaries between the ages of 75 and 84 and over 85 were more likely to develop corneal edema. Asian, Hispanic and North American Native race were associated with increased likelihood of developing corneal edema, and North American Native beneficiaries had higher risk of requiring corneal transplantation compared to white beneficiaries. Female sex decreased the likelihood of requiring corneal transplantation postoperatively, but this may be related to other factors such as higher usage of eyecare services by women.
Understandably, the researchers noted in their paper on the work for American Journal of Ophthalmology, complex cataract procedures were associated with a higher risk of both corneal edema and requiring corneal transplantation.
“Corneal endothelial cell count is known to decrease with age, making older individuals more susceptible to irreversible corneal decompensation following intraocular surgery that may further compromise endothelial integrity,” the authors wrote. ”The mechanism behind the racial difference is less clear, and the effect sizes seen in our study are larger than those previously reported for racial associations with other cataract surgery complications. One could posit that genetic variability may partially contribute to this discrepancy. However, a large-scale analysis of donor corneas found that corneas from Black and Asian patients had higher endothelial cell densities compared to corneas from white patients.”
There was an 0.33% incidence of corneal edema in beneficiaries without diabetes vs. 0.43% incidence in beneficiaries with diabetes.
“While there was no difference in the average time to development of either corneal edema or receiving a corneal transplant in diabetics versus non-diabetics, amongst those with diabetes, macular edema was an independent predictor of corneal edema,” the authors noted.
“While the time to developing corneal edema was similar in diabetic and non-diabetic patients, both groups exhibited large standard deviations attributable to a substantial number of early postoperative cases and instances of late onset,” the authors continued. “This temporal pattern and wide dispersion align with previous studies, which indicate an average duration of eight to nine months for the development of corneal edema. We found a shorter time to corneal transplantation compared to a 1997 report, which may be attributable to improved eye banking infrastructure, increased graft supply and possibly lower threshold for surgical intervention in our date range.”
There was an increased risk of postoperative corneal edema in beneficiaries with proliferative diabetic retinopathy (DR), but no substantial associations were observed with the extent of non-proliferative DR, presence of diabetic macular edema or diabetic kidney disease, possibly due to the increased inflammatory burden and advanced glycation end-product deposition in the aqueous humor associated with proliferative DR compared to no-proliferative DR, the researchers explained.
“In conclusion, though the observed rates of corneal edema following cataract surgery are relatively low, this is the first large-scale study to reveal a complex picture of pseudophakic bullous keratopathy that is influenced by demographic factors such as age, race/ethnicity and gender. Racial/ethnic disparities, particularly the increased likelihood of corneal edema among minoritized populations, raise important questions about healthcare utilization, socioeconomic factors and the late presentation of advanced cataracts,” the authors concluded in their AJO paper.
Li G, Sommi A, Klawe J, Ahmad S. Demographic and systemic risk factors for persistent corneal edema following cataract surgery in patients with and without diabetes. May 20, 2024. [Epub ahead of print.] |


