 |
|
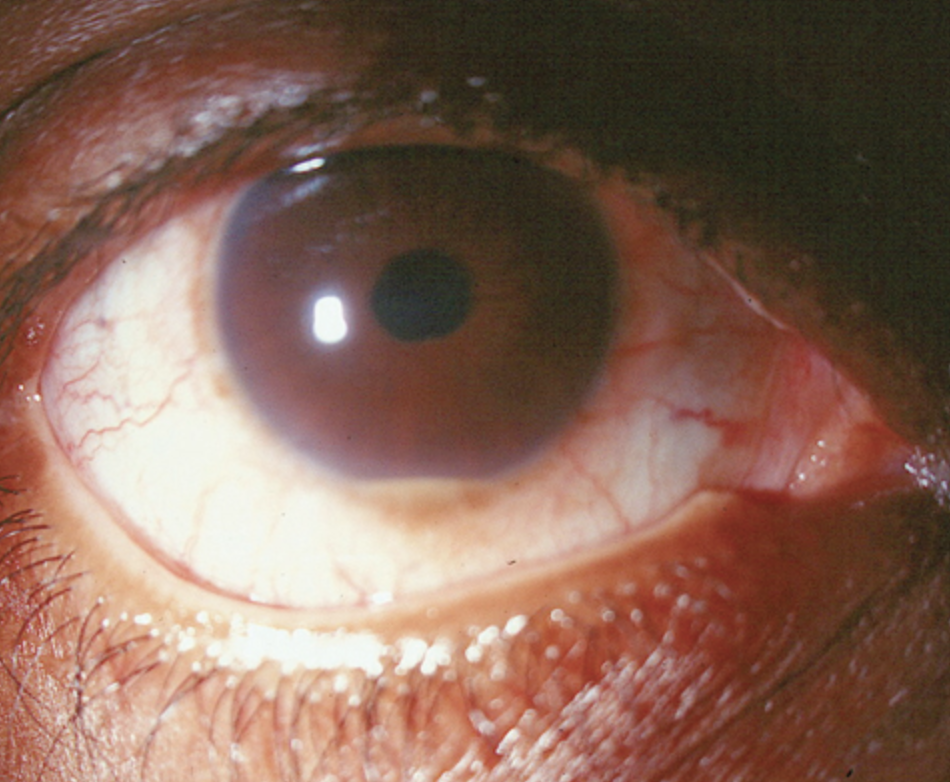
A genetic decrease in vitamin D was associated with an approximately two-fold increase in risk in uveitis and scleritis. Photo: Joseph W. Sowka, OD, and Alan G. Kabat, OD. Click image to enlarge. |
Low genetic vitamin D levels have been associated with immunological dysregulation and autoimmune disorders, as 25-hydroxy vitamin D produced in the liver inhibits the creation of Th1 and Th17 cytokines in the adaptive immune response. Recently, non-infectious uveitis and scleritis, two ocular manifestations of immunological dysregulation, were found to be associated with low vitamin D levels as well in a Mendelian randomization study.
Mendelian randomization uses genetic variants to determine whether an observational association is consistent with a causal effect. In the two-sample Mendelian randomization case-control study presented in American Journal of Ophthalmology, the researchers examined 375 cases of non-infectious uveitis and/or scleritis and 4,167 controls from an academic health care system’s biobank. They reported an association of genetically decreased 25-hydroxy vitamin D with uveitis and scleritis risk (odds ratio 2.16).
The first sensitivity analysis that excluded genetic variants unlikely to have a role on biologically active 25-hydroxy vitamin D found that effect estimates were consistent with those of the primary analysis. A second sensitivity analysis using only the six variants within the CYP2R1 locus found that genetically decreased 25OHD was strongly associated with increased uveitis and scleritis risk. (The CYP2R1converts locus encodes 25-hydroxy vitamin D hydroxylase, a liver enzyme that converts vitamin D to 25-hydroxy vitamin D).
“Our study demonstrated that a genetic decrease in vitamin D was associated with an approximately two-fold increase in risk in uveitis and scleritis,” the researchers explained in their paper. They calculated the mean log 25-hydroxy vitamin D level in their study population to estimate the clinical implications of their findings; they reported a causal effect estimate showing that raising the total 25-hydroxy vitamin D levels from 21ng/mL to 31ng/mL would reduce the risk of uveitis and scleritis by about half.
“A daily supplement of vitamin D3 1,000 units is expected to raise 25-hydroxy vitamin D levels by 6ng/mL to 10ng/mL,” they wrote. “Hence, treating a population that is vitamin D deficient (total 25-hydroxy vitamin D <20ng/mL) to sufficient levels (≥30ng/mL) through vitamin D supplementation, optimizing dietary intake of vitamin D or sun exposure is expected to lower the risk of uveitis by about 50%.”
They pointed out that identifying 25-hydroxy vitamin D as a causal susceptibility factor for ocular inflammation is key since vitamin D deficiency is widespread and supplementation is relatively safe and cost-effective.
Susarla G, Chan W, Li A, et al. Mendelian randomization shows a causal effect of low vitamin D on non-infectious uveitis and scleritis risk. Am J Ophthalmol. 2022. August 7, 2022. [Epub ahead of print]. |


